- Hereditary coproporphyria
-
Hereditary coproporphyria Classification and external resources 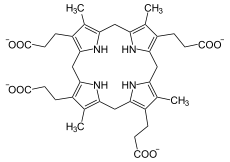
Coproporphyrinogen IIIICD-10 E80.2 (ILDS E80.222) ICD-9 277.1 OMIM 121300 DiseasesDB 30591 eMedicine med/1888 MeSH D046349 Hereditary coproporphyria (HCP) is a type of acute porphyria[1] (formerly categorized as a form of hepatic porphyria) that is associated with a deficiency of the enzyme coproporphyrinogen III oxidase.[2][3]:525
Hereditary coproporphyria (HCP) is an autosomal dominant[4] genetic disease that causes purple urine, photosensitivity, and attacks of abdominal pain. Symptoms vary from mild to severe and can be regulated with diet and triggered with drug use.[5]
It has a prevalence estimated at approximately 1 in 500,000.[6]
Contents
Signs and symptoms
Signs and symptoms of an acute attack involve neurological dysfunction. Areas affected include the gastrointestinal tract resulting in extreme abdominal pain, vomiting, and constipation. Neurological dysfunction can be seen in the cardiovascular system as tachycardia and hypertension. There may also be pain in the extremities, muscle weakness, and sensory loss. [7] Some may have psychological symptoms ranging from agitation to hallucinations.[8] Urine may immediately have a reddish, brownish or purple coloring. However, others may not show this color change unless the urine is exposed to light for 30 minutes.[9]
Around 30% suffer photosensitive skin eruptions with nail involvement; these can lead to permanent scarring.
Attacks of coproporphyria can be life-threatening and should be dealt with accordingly. Treatment is the same as for acute Intermittent and variegate porphyria. See Wikipedia article porphyria for detailed information.
Triggers vary, but infections, hormonal changes, dieting, and the use of alcohol and certain drugs such as barbiturates and hormonal contraceptives have all been implicated.
Cause
HCP is an autosomal disease, meaning it is carried in one of the autosomes, or non-sex chromosomes.[10] There have been documented cases of both heterozygous and homozygous inheritance, with similar symptoms in each patient.[10]
Triggers of acute attacks
Acute attacks of porphyria can be induced by many drugs. The types of drugs may include but are not limited to progesterone, sulfonamides, anti-convulsants, steroids, and barbiturates.[11] Cases noted hereditary coproporphyria induced by methandrostenolone (Dianabol).[12] For more complete listings of drugs that may induce acute attacks, there are a number of online resources that may be referenced. These include NAPOS (the Norwegian Porphyria Centre), Porphyria South Africa, and http://www.porphyriafoundation.com/drug-database. All three databases have drugs listed in English. The Norwegian Porphyria Centre's list is also available in French and Swedish.
Pathophysiology
Hereditary coproporphyria is the result of a point mutation in the coproporphinogen oxidase (CPO) gene.[10][13] Documented changes in the DNA sequence that cause HCP include missense, nonsense, deletion and splicing of single nucleotides.[10][14] Documented changes in the protein sequence have been a replacement of ser208 to phe(s208f) and arg328 to cys(r328c).[10] Aside from varying intensity of symptoms there are no other known mutations, and it is not known at this time if mutations in other genes can trigger this same disease. At this time it is not known if there are any specific groups of people that are especially susceptible to this disease, as patients have been documented all over the world.
Molecular biology
The CPO gene is located in chromosome 3 on the q12 locus.[10] The gene is 14,000 bases in length, has 6 introns, and 7 exons. Once the introns are spliced out the actual coded mRNA is only 2675 bases in length.[15] The protein contains 323 amino acids.
Function
The coproporphinogen oxidase gene is an enzyme expressed in erythrocytes that converts coproporphyrinogen III to protoporphyrinogen IX.[10] Heme is made from porphyrin and when a mutation occurs, heme production is interrupted. This leads to an overabundance of porphyrin in the body, which then exits through urine/feces.[5]
Treatment
While there is no cure for this condition, there are preventative measures people can take to regulate symptoms. A diet high in carbohydrates, glucose, as well as avoidance of aggravating factors (such as alcohol and drug use) can prevent attacks.[5]
See also
References
- ^ Stig Thunnell, MD PhD. "Acute Porphyrias". http://www.merckmanuals.com/professional/endocrine_and_metabolic_disorders/porphyrias/acute_porphyrias.html. Retrieved 2011-04-09.
- ^ Schmitt C, Gouya L, Malonova E et al. (October 2005). "Mutations in human CPO gene predict clinical expression of either hepatic hereditary coproporphyria or erythropoietic harderoporphyria". Hum. Mol. Genet. 14 (20): 3089–98. doi:10.1093/hmg/ddi342. PMID 16159891. http://hmg.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16159891.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ^ Wiman A, Floderus Y, Harper P (2002). "Two novel mutations and coexistence of the 991C>T and the 1339C>T mutation on a single allele in the coproporphyrinogen oxidase gene in Swedish patients with hereditary coproporphyria". J. Hum. Genet. 47 (8): 407–12. doi:10.1007/s100380200059. PMID 12181641.
- ^ a b c MedicineNet.com. "Porphyria". http://www.medterms.com/script/main/art.asp?articlekey=10360. Retrieved 2007-12-07.
- ^ Arceci, Robert.; Hann, Ian M.; Smith, Owen P. (2006). Pediatric hematolog. Malden, Mass.: Blackwell Pub.. ISBN 978-1-4051-3400-2.
- ^ Lancet. 1997 May 31;349(9065):1613-7. The acute porphyrias. Elder GH, Hift RJ, Meissner PN.
- ^ Santosh PJ, Malhotra S: Varied psychiatric manifestations of acute intermittent porphyria. Biol Psychiatry 1994; 744–777
- ^ Thunell, Stig, MD, PhD (August 2008). Acute Intermittent Porphyria. Merck Manuals Online Medical Library. Merck Sharp & Dohme Corp., as subsidiary of Merck & Co., Inc. http://www.merckmanuals.com/professional/endocrine_and_metabolic_disorders/porphyrias/overview_of_porphyrias.html Retrieved 5 February 2011.
- ^ a b c d e f g Online 'Mendelian Inheritance in Man' (OMIM) Coproporphyria -121300
- ^ Thunell, Stig, MD, PhD (August 2008). Acute Intermittent Porphyria. Merck Manuals Online Medical Library. Merck Sharp & Dohme Corp., as subsidiary of Merck & Co., Inc. http://www.merckmanuals.com/home/hormonal_and_metabolic_disorders/porphyrias/acute_intermittent_porphyria.html Retrieved 5 February 2011.
- ^ http://www.eblue.org/article/S0190-9622(94)70029-X/abstract
- ^ Lee DS, Demeler B, sek P, Flachsová E, Bodnárová M, Martá Raman CS, Martásek, P, Raman, CS (October 2005). "Structural basis of hereditary coproporphyria". Proc. Natl. Acad. Sci. U.S.A. 102 (40): 14232–7. doi:10.1073/pnas.0506557102. PMC 1224704. PMID 16176984. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=16176984.
- ^ Rosipal R, Lamoril J, Puy H et al. (1999). "Systematic analysis of coproporphyrinogen oxidase gene defects in hereditary coproporphyria and mutation update". Hum. Mutat. 13 (1): 44–53. doi:10.1002/(SICI)1098-1004(1999)13:1<44::AID-HUMU5>3.0.CO;2-Q. PMID 9888388.
- ^ GenBank. "Coproporphyrinogen Oxidase". http://www.ncbi.nlm.nih.gov/entrez/viewer.fcgi?db=nucleotide&val=33991442. Retrieved 2007-12-07.
External links
- Porphyria at NLM Genetics Home Reference
- Coproporphyria at NIH's Office of Rare Diseases
- MedlinePlus Encyclopedia Porphyria
Heme metabolism disorders (E80, 277.1, 277.4) Porphyria,
hepatic and erythropoietic
(porphyrin)Hereditary hyperbilirubinemia
(bilirubin)Categories:- Porphyrias
- Skin conditions resulting from errors in metabolism
Wikimedia Foundation. 2010.
