- Dental restoration
-
Dental restoration Intervention ICD-9-CM 23.2-23.4 A dental restoration or dental filling is a dental restorative material used to restore the function, integrity and morphology of missing tooth structure. The structural loss typically results from caries or external trauma. It is also lost intentionally during tooth preparation to improve the aesthetics or the physical integrity of the intended restorative material. Dental restoration also refers to the replacement of missing tooth structure that is supported by dental implants.
Dental restorations can be divided into two broad types: direct restorations and indirect restorations. All dental restorations can be further classified by their location and size. A root canal filling is a restorative technique used to fill the space where the dental pulp normally resides.
Contents
Tooth preparation
 Tooth #3, the upper right first molar, with the beginning of an MO preparation. Looking into the preparation, the white, outer enamel appears intact, while the yellow, underlying dentin appears recessed. This is because the dentin was decayed and was thus removed. This portion of the enamel is now unsupported, and should be removed to prevent future fracture.
Tooth #3, the upper right first molar, with the beginning of an MO preparation. Looking into the preparation, the white, outer enamel appears intact, while the yellow, underlying dentin appears recessed. This is because the dentin was decayed and was thus removed. This portion of the enamel is now unsupported, and should be removed to prevent future fracture.
Restoring a tooth to good form and function requires two steps, (1) preparing the tooth for placement of restorative material or materials, and (2) placement of restorative material or materials.
The process of preparation usually involves cutting the tooth with special dental burrs, to make space for the planned restorative materials, and to remove any dental decay or portions of the tooth that are structurally unsound. If permanent restoration can not be carried out immediately after tooth preparation, temporary restoration may be performed.
The prepared tooth, ready for placement of restorative materials, is generally called a tooth preparation. Materials used may be gold, amalgam, dental composites, resin-reinforced glass ionomers, porcelain or any number of other materials.
Preparations may be intracoronal or extracoronal.
- Intracoronal preparations are those preparations which serve to hold restorative material within the confines of the structure of the crown of a tooth. Examples include all classes of cavity preparations for composite or amalgam, as well as those for gold and porcelain inlays. Intracoronal preparations are also made as female recipients to receive the male components of Removable partial dentures.
- Extracoronal preparations are those preparations which serve as a core or base upon which or around which restorative material will be placed to bring the tooth back into a functional or aesthetic structure. Examples include crowns and onlays, as well as veneers.
In preparing a tooth for a restoration, a number of considerations will come into play to determine the type and extent of the preparation. The most important factor to consider is decay. For the most part, the extent of the decay will define the extent of the preparation, and in turn, the subsequent method and appropriate materials for restoration.
Another consideration is unsupported tooth structure. In the photo at right, unsupported enamel can be seen where the underlying dentin was removed because of infiltrative decay. When preparing the tooth to receive a restoration, unsupported enamel is removed to allow for a more predictable restoration. While enamel is the hardest substance in the human body, it is particularly brittle, and unsupported enamel fractures easily.
Direct restorations
This technique involves placing a soft or malleable filling into the prepared tooth and building up the tooth before the material sets hard. The advantage of direct restorations is that they usually set quickly and can be placed in a single procedure. Since the material is required to set while in contact with the tooth, limited energy can be passed to the tooth from the setting process without damaging it. Where strength is required, especially as the fillings become larger, indirect restorations may be the best choice.
Indirect restorations
This technique of fabricating the restoration outside of the mouth using the dental impressions of the prepared tooth. Common indirect restorations include inlays and onlays, crowns, bridges, and veneers. Usually a dental technician fabricates the indirect restoration from records the dentist has provided of the prepared tooth. The finished restoration is usually bonded permanently with a dental cement. It is often done in two separate visits to the dentist. Common indirect restorations are done using gold or ceramics.
While the indirect restoration is being prepared, a provisory/temporary restoration is sometimes used to cover the prepared part of the tooth, which can help maintain the surrounding dental tissues.
Removable dental prostheses (mainly dentures) are considered by some to be a form of indirect dental restoration, as they are made to replace missing teeth. There are numerous types of precision attachments (also known as combined restorations) to aid removable prosthetic attachment to teeth, including magnets, clips, hooks and implants which could be seen as a form of dental restoration.
The CEREC method is a chairside CAD/CAM restorative procedure. An optical impression of the prepared tooth is taken using a camera. Next, the specific software takes the digital picture and converts it into a 3D virtual model on the computer screen. A ceramic block that matches the tooth shade is placed in the milling machine. An all-ceramic, tooth-colored restoration is finished and ready to bond in place.
Another fabrication method is to import STL and native dental CAD files into CAD/CAM software products that guide the user through the manufacturing process. The software can select the tools, machining sequences and cutting conditions optimized for particular types of materials, such as titanium and zirconium, and for particular prostheses, such as copings and bridges. In some cases, the intricate nature of some implants requires the use of 5-axis machining methods to reach every part of the job.[1]
Restoration classifications
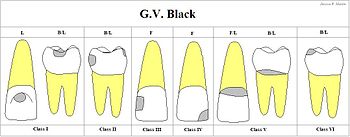
Greene Vardiman Black classified the fillings depending on their size and location.[2]
- Class I Caries affecting pit and fissure, on occlusal, buccal, and lingual surfaces of posterior teeth, and Lingual of anterior teeth.
- Class II Caries affecting proximal surfaces of molars and premolars.
- Class III Caries affecting proximal surfaces of centrals, laterals, and cuspids.
- Class IV Caries affecting proximal including incisal edges of anterior teeth.
- Class V Caries affecting gingival 1/3 of facial or lingual surfaces of anterior or posterior teeth.
- Class VI Caries affecting cusp tips of molars, premolars, and cuspids.
Materials used in dental restorations
These metals are mostly used for making crowns, bridges and dentures. Pure titanium could be successfully incorporated into bone. It is biocompatible and stable.
- Precious metallic alloys
- gold (high purity: 99.7%)
- gold alloys (with high gold content)
- gold-platina alloy
- silver-palladium alloy
- titanium
- Base metallic alloys
- Amalgam
- Silver amalgam
Amalgam is widely used for direct fillings, mainly for posterior teeth, and completed in single appointment. Cast gold is used for indirect restorations. Amalgam leaches tiny amounts of mercury and while some concerns have been raised, there is currently no evidence that any of this mercury remains in the body nor that dangerous levels are ever reached.[3]
- Direct Gold
- Gold
Although rarely used, due to expense and specialized training requirements, gold foil can be used for direct dental restorations.
Tooth colored
Dental composites are also called white fillings, used in direct fillings. Crowns and in-lays can be made in the laboratory from dental composites. These materials are similar to those used in direct fillings and are tooth coloured. Their strength and durability is not as high as porcelain or metal restorations and they are more prone to wear and discolouration.
Composite resin
Dental composites, also called white fillings, are a group of restorative materials used in dentistry. As with other composite materials, a dental composite typically consists of a resin-based matrix, such as a bisphenol A-glycidyl methacrylate (BISMA) resin like urethane dimethacrylate (UDMA), and an inorganic filler such as silicon dioxide silica. Compositions vary widely, with proprietary mixes of resins forming the matrix, as well as engineered filler glasses and glass ceramics. The filler gives the composite wear resistance and translucency. A coupling agent such as silane is used to enhance the bond between these two components. An initiator package begins the polymerization reaction of the resins when external energy (light/heat, etc.) is applied. A catalyst package can control its speed. This is not recommended for molars[citation needed].
After tooth preparation, a thin glue or bonding material layer is applied. Composites are then filled layer by layer and photo-polymerising each using light.[4] At the end the surface will be shaped and polished.
Glass ionomer cement
A glass ionomer cement (GIC) is one of a class of materials commonly used in dentistry as filling materials and luting cements. These materials are based on the reaction of silicate glass powder and polyalkeonic acid. These tooth-coloured materials were introduced in 1972 for use as restorative materials for anterior teeth (particularly for eroded areas, Class III and V cavities).
As they bond chemically to dental hard tissues and release fluoride for a relatively long period, modern-day applications of GICs have expanded. The desirable properties of glass ionomer cements make them useful materials in the restoration of carious lesions in low-stress areas such as smooth-surface and small anterior proximal cavities in primary teeth. Results from clinical studies also support the use of conventional glass ionomer restorations in primary molars. They need not be put in layer by layer, like in composite fillings.
Porcelain (ceramics)
Full-porcelain (ceramic) dental materials include porcelain, ceramic or glasslike fillings and crowns (a.k.a jacket crown, as a metal-free option). They are used as in-lays, on-lays, crowns, and aesthetic veneers. A veneer is a very thin shell of porcelain that can replace or cover part of the enamel of the tooth. Full-porcelain (ceramic) restorations are particularly desirable because their color and translucency mimic natural tooth enamel.
Another type is known as porcelain-fused-to-metal, which is used to provide strength to a crown or bridge. These restorations are very strong, durable and resistant to wear, because the combination of porcelain and metal creates a stronger restoration than porcelain used alone.
One of the advantages of computerized dentistry (CAD/CAM technologies) is that it enabled the application of zirconium-oxide (ZrO2). The introduction of this material in restorative and prosthetic dentistry is most likely the decisive step toward the use of full ceramics without limitation. With the exception of zirconium-oxide, existing ceramics systems lack reliable potential for the various indications for bridges without size limitations. Zirconium-oxide with its high strength and comparatively higher fracture toughness seems to buck this trend. With a three-point bending strength exceeding 900 megapascals, zirconium-oxide can be used in virtually every full ceramic prosthetic solution, including bridges, implant supra structures and root dowel pins.
Previous attempts to extend its application to dentistry were thwarted by the fact that this material could not be processed using traditional methods used in dentistry. The arrival of computerized dentistry enables the economically prudent use of zirconium-oxide in such elements as base structures such as copings and bridges and implant supra structures. Special requirements apply to dental materials implanted for longer than a period of thirty days. Several technical requirements include high strength, corrosion resistance and defect-free producibility at a reasonable price.
Ever more stringent requirements are being placed on the aesthetics of teeth. Metals and porcelain are currently the materials of choice for crowns and bridges. The demand for full ceramic solutions, however, continues to grow. Consequently, industry and science are increasingly compelled to develop full ceramic systems. In introducing full ceramic restorations, such as base structures made of sintered ceramics, computerized dentistry plays a key role.
Comparison
- Composites and Amalgam are used mainly for direct restoration. Composites can be made of color matching the tooth, and surface can be polished after filling.
- Amalgam fillings expand with age, possibly cracking the tooth and requiring repair and filling replacement. But chance of leakage of filling is less.
- Composite fillings shrink with age and may pull away from the tooth allowing leakage. If leakage is not noticed early recurrent decay may occur.
- Fillings have a finite lifespan: an average of 12.8 years for amalgam and 7.8 years for composite resins.[5] Fillings fail because of changes in the filling, tooth or the bond between them. Secondary caries formation can also affect the structural integrity the original filling. Fillings are recommended for small to medium sized restorations.
- Porcelain and Gold are used for indirect restorations like crowns and partial coverage crowns (onlays). Some types of porcelains are hard, but can cause wear on opposing teeth. They are brittle and are not always recommended for molar restorations. A new material called lithium disilicate (ips.emax) is indicated for use on molars for crowns and onlays now because it is fracture resistant compared to other porcelains used for dental restorations.[6]
Experimental
In 2010, researchers reported that they were able to stimulate mineralization of an enamel-like layer of fluorapatite in vivo.[7]
Restoration of dental implants
Dental implants, are anchors placed in bone, usually made from titanium or titanium alloy. They can support dental restorations which replace missing teeth. Some restorative applications include supporting crowns, bridges, or dental prostheses.
See also
- Dental restorative materials the materials used for fillings
- CEREC
- Fixed prosthodontics
- Dental treatment
- Dental dam
- Gold teeth
- CAD/CAM Dentistry
- Treatment of knocked-out (avulsed) teeth
- Triodent V3 Sectional Matrix System for Class II restorations
References
- ^ TCT magazine, “WorkNC Dental at the "CAD/CAM and Rapid Prototyping in Dental Technology" conference”
- ^ G. V. Black Classification of Carious Lesions
- ^ http://www.ada.org/sections/publicResources/pdfs/dental_fillings_facts_full.pdf
- ^ Canadian Dental Association, Tooth-coloured fillings
- ^ Van Nieuwenhuysen JP, D'Hoore W, Carvalho J, Qvist V. Long-term evaluation of extensive restolihnlknudy assessed the outcome of posterior extensive restorations and identified risk factors for failure of the restorations. ... The Kaplan–Meier median survival times were 12.8 years for amalgam restorations, 7.8 years for resin restorations, and more than 14.6 years for crowns, considering all retreatment as failures (P=0.002).
- ^ Christian F.J. Stappert, Wael Att, Thomas Gerds, and Joerg R. Strub Fracture resistance of different partial-coverage ceramic molar restorations: An in vitro investigation J Am Dent Assoc 2006 137: 514-522.
- ^ Guentsch et al. (2010). Biomimetic Mineralization: Effects on Human Enamel In Vivo. Advanced Engineering Materials.
External links
- How Dental Restoration Materials Compare
- Triodent's V3 Sectional Matrix System
- Gold Foil In Dentistry
Prosthodontology (ICD-9-CM V3 23.2-23.6, ICD-10-PCS 0C?W-X) Fixed Prosthodontic Restorations Dental restoration: Bridge (Resin retained bridge, Rochette bridge) - Crown (Post and core) - Inlays and onlays - Veneer
Diagnostic wax-upRemovable Prosthodontic Restorations Prosthodontic considerations Maxillofacial Prosthodontics Other specialties
See alsoCategories:- Dental materials
- Dentistry procedures
- Restorative dentistry
Wikimedia Foundation. 2010.