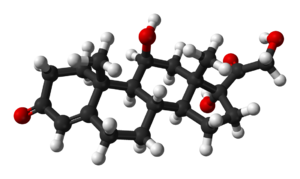
- Cortisol awakening response
-
The cortisol awakening response (CAR) is an increase of about 50% in cortisol levels occurring 20–30 minutes after awakening in the morning in some people. This rise is superimposed upon the late-night rise in cortisol which occurs before awakening. It is thought to be linked to the hippocampus' preparation of the hypothalamic-pituitary-adrenal axis (HPA) to face anticipated stress.
Contents
Description
Shortly after awakening, a sharp 38–75% (average 50%) increase occurs in the blood level of cortisol in about 77%[1] of healthy adults, and it occurs in people of all ages.[2] The average level of cortisol upon waking is roughly 15 nmol/l; 30 minutes later it may be 23 nmol/l, though there are wide variations.[1] The cortisol awakening response reaches a maximum approximately 30 minutes after awakening though it may still be heightened by 34% an hour after waking.[1] The pattern of this response to waking is relatively stable for any individual.[3][1] Twin studies show its pattern is largely genetically determined since there is a heritability of 0.40 for the mean cortisol increase after awakening and 0.48 for the area under the cortisol rise curve.[4]
Normally, the highest cortisol secretion happens in the second half of the night with peak cortisol production occurring in the early morning. Following this, cortisol levels decline throughout the day with lowest levels during the first half of the night.[5] Cortisol awakening response is independent of this circadian variation in HPA axis activity; it is superimposed upon the daily rhythm of HPA axis activity; and it seems to be linked specifically to the event of awakening.[6]
Cortisol awakening response provides an easy measure of the reactivity capacity of the HPA axis.[7]
Sleep factors
- Waking up earlier in the morning increases the response.[8]
- Shift work: nurses working on morning shifts with very early awakening (between 4:00–5:30 a.m.) had a greater and prolonged cortisol awakening response than those on the late day shift (between 6:00–9:00 a.m.) or the night shift (between 11:00 a.m.–2:00 p.m.).[9] However another study found this attributed this greater respose to increased stress and impaired sleep quality before an early work shift.[10]
- Naps: students taking a nap of one to two hours in the early evening hours (between 6:45–8:30 p.m.) had no cortisol awakening response, suggesting cortisol awakening response only occurs after night sleep.[9]
- Waking up in the light: cortisol awakening response is larger when people wake up in light rather than darkness.[11][12]
- Noise: there is no cortisol rise after nights with traffic-like low-frequency noise.[13]
- Alarm clock vs. spontaneous waking: there is no difference on days when people woke up spontaneously or used the alarm clock.[1]
- Aspirin has been found to reduce the response probably through an action upon ACTH.[14]
Individual factors
- Morning types show a larger cortisol awakening response than evening types.[15]
- Those suffering fatigue show a low rise and flat plateau.[16]
- Those in pain: the response is reduced the more people are in pain.[17]
- The lower a person's socioeconomic status, the higher their response.[18] This might link to the material hardship that occurs with low socioeconomic status.[19]
Stress
Cortisol awakening response is larger for those:
- waking up to a working day compared to work-free weekend day.[20][21]
- experiencing chronic stress and worry[21][4]
- overloaded with work.[22]
- in acute stress. People taking part in a competitive ballroom dance tournament had an increased cortisol awakening response on the morning of their competition day but not their non-competition one.[23]
- worn down by burnout: some studies find an increased[24][25] though other researchers find a decreased[26] or normal response.[27]
Neurology
Cortisol is released from the adrenal glands following activation by ACTH release from the pituitary. The ACTH release creating the cortisol awakening response is strongly inhibited after intake of a low-dose dexamethasone.[28] This is a synthetic glucocorticoid and this inhibition allows the detection of the presence of negative feedback from circulating cortisol that controls to ACTH-secreting cells of the pituitary.
In the hypothalamic-pituitary-adrenal axis the pituitary release of ACTH is regulated by the hypothalamus. In the cortisol awakening response, the hypothalamic-pituitary-adrenal axis is controlled by the hippocampus. For example, cortisol awakening response is absent in those with bilateral and unilateral hippocampus damage[29] and hippocampal atrophy.[30] Those with severe amnesia, and thus with presumed damage to the temporal lobe, also do not have it.[31] Those with a larger hippocampus have a greater response.[32]
It plausible also that the suprachiasmatic nucleus, the light-sensitive biological clock, plays a role in cortisol awakening response regulation.[2]
Function
The function of cortisol awakening response is unknown but it has been suggested to link with a stress-related preparation in regard to the upcoming day by the hippocampus. One hypothesis is: "that the cortisol rise after awakening may accompany an activation of prospective memory representations at awakening enabling individual's orientation about the self in time and space as well as anticipation of demands of the upcoming day... it is tempting to speculate that for the CAR, anticipation of these upcoming demands may be essential in regulating the CAR magnitude for the particular day. The hippocampus is, besides its established role in long-term memory consolidation, involved in the formation of a cohesive construct and representation of the outside world within the central nervous system processing information about space, time and relationships of environmental cues. This puts the hippocampus in a pivotal position for the regulation of the CAR."[2]
See also
References
- ^ a b c d e Wüst S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. (2000).The cortisol awakening response – normal values and confounds. Noise Health. 2(7):79-88. PMID 12689474
- ^ a b c Fries E, Dettenborn L, Kirschbaum C. (2009). The cortisol awakening response (CAR): facts and future directions. Int J Psychophysiol. 72(1):67–73. PMID 18854200
- ^ Hucklebridge F, Hussain T, Evans P, Clow A. (2005). The diurnal patterns of the adrenal steroids cortisol and dehydroepiandrosterone (DHEA) in relation to awakening. Psychoneuroendocrinology. 30(1):51–7. PMID 15358442
- ^ a b Wüst S, Federenko I, Hellhammer DH, Kirschbaum C. (2000). Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 25(7):707–20. PMID 10938450
- ^ Tsigos C, Chrousos GP. (2002). Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J Psychosom Res. 53(4):865–71. doi:10.1016/S0022-3999(02)00429-4 PMID 12377295
- ^ Wilhelm I, Born J, Kudielka BM, Schlotz W, Wüst S. (2007). Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 32(4):358–66. PMID 17408865
- ^ Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schürmeyer TH, Kirschbaum C. (1999). The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 64(18):1653–60. PMID 10328525
- ^ Kudielka BM, Kirschbaum C. (2003). Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology. 28(1):35–47. PMID 12445835
- ^ a b Federenko I, Wüst S, Hellhammer DH, Dechoux R, Kumsta R, Kirschbaum C. (2004) Free cortisol awakening responses are influenced by awakening time. Psychoneuroendocrinology. 29(2):174–84. PMID 14604599
- ^ Williams E, Magid K, Steptoe A. (2005). The impact of time of waking and concurrent subjective stress on the cortisol response to awakening. Psychoneuroendocrinology. 30(2):139–48. PMID 15471612
- ^ Scheer FA, Buijs RM. (1999). Light affects morning salivary cortisol in humans. J Clin Endocrinol Metab. 84(9):3395–8. PMID 10487717
- ^ Thorn L, Hucklebridge F, Esgate A, Evans P, Clow A. (2004). The effect of dawn simulation on the cortisol response to awakening in healthy participants. Psychoneuroendocrinology. 29(7):925–30. PMID 15177708
- ^ Waye KP, Clow A, Edwards S, Hucklebridge F, Rylander R. (2003). Effects of nighttime low frequency noise on the cortisol response to awakening and subjective sleep quality. Life Sci. 72(8):863–75. PMID 12493567
- ^ Watson S, Horton K, Bulmer S, Carlile J, Corcoran C, Gallagher P, Ferrier IN. (2009). Effect of aspirin on hypothalamic-pituitary-adrenal function and on neuropsychological performance in healthy adults: a pilot study.Psychopharmacology (Berl). 205(1):151–5. PMID 19404617
- ^ Kudielka BM, Federenko IS, Hellhammer DH, Wüst S. (2006). Morningness and eveningness: the free cortisol rise after awakening in "early birds" and "night owls". Biol Psychol. 72(2):141–6. PMID 16236420
- ^ Kumari M, Badrick E, Chandola T, Adam EK, Stafford M, Marmot MG, Kirschbaum C, Kivimaki M. (2009). Cortisol secretion and fatigue: Associations in a community based cohort. Psychoneuroendocrinology. PMID 19497676
- ^ Fabian LA, McGuire L, Page GG, Goodin BR, Edwards RR, Haythornthwaite J. (2009). The association of the cortisol awakening response with experimental pain ratings. Psychoneuroendocrinology. 34(8):1247–51. PMID 19375866
- ^ Wright CE, Steptoe A. (2005). Subjective socioeconomic position, gender and cortisol responses to waking in an elderly population. Psychoneuroendocrinology. 30(6):582–90. PMID 15808928
- ^ Ranjit N, Young EA, Kaplan GA. (2005). Material hardship alters the diurnal rhythm of salivary cortisol. Int J Epidemiol. 34(5):1138–43. PMID 15951357
- ^ Thorn L, Hucklebridge F, Evans P, Clow A. (2006). Suspected non-adherence and weekend versus week day differences in the awakening cortisol response. Psychoneuroendocrinology. 31(8):1009–18. PMID 16876958
- ^ a b Schlotz W, Hellhammer J, Schulz P, Stone AA. (2004). Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom Med. 66(2):207–14. PMID15039505
- ^ Steptoe A, Cropley M, Griffith J, Kirschbaum C. (2000). Job strain and anger expression predict early morning elevations in salivary cortisol. Psychosom Med. 62(2):286–92. PMID 10772410
- ^ Rohleder N, Beulen SE, Chen E, Wolf JM, Kirschbaum C. (2007). Stress on the dance floor: the cortisol stress response to social-evaluative threat in competitive ballroom dancers. Pers Soc Psychol Bull. 33(1):69–84. PMID 17178931
- ^ Grossi G, Perski A, Ekstedt M, Johansson T, Lindström M, Holm K. (2005). The morning salivary cortisol response in burnout. J Psychosom Res. 59(2):103–11. PMID 16186006
- ^ De Vente W, Olff M, Van Amsterdam JG, Kamphuis JH, Emmelkamp PM. (2003). Physiological differences between burnout patients and healthy controls: blood pressure, heart rate, and cortisol responses. Occup Environ Med. 60 Suppl 1:i54–61. PMID 12782748
- ^ Pruessner JC, Hellhammer DH, Kirschbaum C. (1999). Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 61(2):197–204. PMID 10204973
- ^ Mommersteeg PM, Heijnen CJ, Verbraak MJ, van Doornen LJ. (2006). Clinical burnout is not reflected in the cortisol awakening response, the day-curve or the response to a low-dose dexamethasone suppression test. Psychoneuroendocrinology. 31(2):216–25. PMID 16150550
- ^ Ehrhart-Bornstein M, Bornstein SR, Scherbaum WA. (1996). Sympathoadrenal system and immune system in the regulation of adrenocortical function. Eur J Endocrinol. 135(1):19–26. PMID 8765968
- ^ Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. (2004). Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry.;56(9):651–6. PMID 15522248
- ^ Bruehl H, Wolf OT, Convit A. (2009). A blunted cortisol awakening response and hippocampal atrophy in type 2 diabetes mellitus. Psychoneuroendocrinology. 34(6):815–21. PMID 19167831
- ^ Wolf OT, Fujiwara E, Luwinski G, Kirschbaum C, Markowitsch HJ. (2005). No morning cortisol response in patients with severe global amnesia. Psychoneuroendocrinology. 30(1):101–5. PMID 15358447
- ^ Pruessner M, Pruessner JC, Hellhammer DH, Bruce Pike G, Lupien SJ. (2007). The associations among hippocampal volume, cortisol reactivity, and memory performance in healthy young men. Psychiatry Res. 155(1):1–10. PMID 17395434
Categories:- Neuroendocrinology
- Sleep physiology
- Unsolved problems in neuroscience
- Stress
Wikimedia Foundation. 2010.