- Medium-chain acyl-coenzyme A dehydrogenase deficiency
-
Medium-chain acyl-coenzyme A dehydrogenase deficiency (MCAD) Classification and external resources ICD-9 277.85 OMIM 201450 eMedicine ped/1392 Medium-chain acyl-coenzyme A dehydrogenase deficiency (MCADD) is a fatty acid oxidation disorder associated with inborn errors of metabolism. It is due to defects in the enzyme complex known as medium-chain acyl dehydrogenase (MCAD) and reduced activity of this complex. This complex oxidizes medium chain fatty acids (Fatty acids having 6-12 carbons) while reducing FAD to FADH2
It is recognized as one of the more rare causes of sudden infant death syndrome (SIDS), although it may be better described as a mimic, rather than a cause, of SIDS.[citation needed]
Contents
Overview
Two main types of fat are found in the body: triglycerides and waxes. A triglyceride consists of a three-carbon compound known as glycerol to which three fatty acids (carboxylic acids) are attached by ester bonds. The length of the fatty acids chains can vary; they may be classified as very long-chain, long-chain, medium-chain or short-chain depending on the number of carbon atoms in the chain.
The fatty acids are broken down in stages by the successive removal of molecules of acetyl-coenzyme A, which contains 2 carbon atoms. Ultimately, under normal conditions, the fatty acids are converted into carbon dioxide and water with the liberation of energy during this process. Once a fatty acid molecule is "activated" (attached to coenzyme A), a series of four reactions, each catalyzed by a different enzyme, is required to remove each acetyl-coenzyme A molecule. As the first step involves removal of hydrogen atoms (i.e. an oxidation) from an acyl group, the enzyme complex is known as an acyl dehydrogenase. Different enzymes are required to hold fatty acids of different lengths, and the deficiencies connected with these various proteins are:
- Very long-chain acyl-coenzyme A dehydrogenase deficiency (VLCAD deficiency)
- Long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency (LCAD deficiency)
- Medium-chain acyl-coenzyme A dehydrogenase deficiency (MCAD deficiency)
- Short-chain acyl-coenzyme A dehydrogenase deficiency (SCAD deficiency)
- 3-hydroxyacyl-coenzyme A dehydrogenase deficiency (M/SCHAD deficiency)
Diagnosis
In individuals that have reduced activity of MCAD, there is an impairment of fatty acid oxidation. Under conditions of health this may not cause significant problems. However, when such individuals do not eat for prolonged periods or have increased energy requirements, the impairment of fatty acid oxidation may lead to fatty acid buildup, hypoglycemia, hyperammonemia, and, possibly, sudden death. First symptoms of such an episode, termed a "metabolic crisis," are vomiting and lethargy, and typically present before the onset of hypoglycemia. 20-25% of undiagnosed cases are fatal, and many survivors are left with severe brain damage after particularly severe crises.
The oxidation of fatty acids occurs within mitochondria. Fatty acids from the cytoplasm are attached to a molecule called carnitine to transport them across the mitochondrial membrane. The combination of carnitine with a fatty acid is known as acyl carnitine. In individuals with MCADD, there is an increase in the concentration of medium-chain acyl carnitines in the cytoplasm of their cells; these acyl carnitines leak into the blood stream. The presence of these acyl carnitines, especially octanoyl-carnitine, is a major diagnostic characteristic of MCADD.[citation needed]
Treatment
There is no cure for MCADD, but once diagnosed, adverse effects can be prevented by proper management. The most important part of treatment is to ensure that patients never go without food for longer than 10–12 hours (a typical overnight fast). Patients with an illness causing loss of appetite or severe vomiting may need intravenous glucose to make sure that the body is not dependent on fatty acids for energy. Patients also usually adhere to a low-fat diet. Patients may also take daily doses of carnitine, which helps reduce toxic accumulation of fatty acids by forming acyl carnitines, which are excreted in the urine. Severity of symptoms seems to decrease after puberty, but crises may be brought about by particularly long fasts or heavy alcohol consumption.
Forensic deliniation
During the course of an investigation of an infant that has died from sudden infant death syndrome, a sample of blood may be taken to measure the concentration of acyl carnitines. MCAD deficiency may be inferred when the levels of acyl carnitines in the blood are raised in a typical pattern.
If the interval between SIDS and post-mortem examination (autopsy) is not too long, it is sometimes possible to culture cells called fibroblasts from the dermis of a sample of skin taken during the course of the examination. It is possible to add fatty acids that contain radioactive carbon atoms (carbon-14) to the culture medium. If the cells oxidise these fatty acids during the course of their metabolism, radioactive carbon dioxide will be produced, which may be detected using suitable apparatus. The rate of production of radioactive carbon dioxide from fatty acid chains of differing lengths may be used as a test to evaluate whether the cells have a deficiency in any of the various acyl dehydrogenases. This type of test may be used to support a diagnosis of MCAD deficiency when it is suspected from the pattern of acyl carnitines in the blood. The diagnosis of MCAD deficiency should also be considered in the presence of prominent fatty change (also known as steatosis) within the liver and proximal renal tubules of the kidney. However, steatosis is recognised as a non-specific response to a variety of injuries.
Genetics
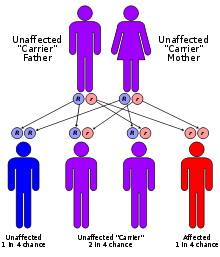
Mutations in the ACADM gene lead to inadequate levels of the medium-chain acyl-coenzyme A dehydrogenase enzyme. This condition is inherited in an autosomal recessive pattern, which means two copies of the faulty gene in each cell are required for the disorder to be inherited. If only one copy of the faulty gene is inherited, the individual is a carrier, but does not have the disorder.
Many mutations have been identified in affected patients, but by far the most common mutation is the A985G mutation, in which an adenine is replaced with a guanine on position 985 of the cDNA. Even among patients homozygous for this mutation, however, there is a wide spectrum of disease severity, ranging from asymptomatic to lethal. In some instances, asymptomatic parents have been diagnosed with MCAD deficiency after a child's diagnosis.
See also
- List of fatty acid metabolism disorders
External links
- Medium-chain acyl-coenzyme A dehydrogenase deficiency at NLM Genetics Home Reference
- CDC
- newbornscreening.info
- Gladwin Medical Blog
- GeneReview/NIH/UW entry on Medium-Chain Acyl-Coenzyme A Dehydrogenase Deficiency
- 422903871 at GPnotebook
Inborn error of lipid metabolism: fatty-acid metabolism disorders (E71.3, 277.81–277.85) Synthesis Degradation Acyl transportGeneralOtherTo acetyl-CoASjögren–Larsson syndromeCategories:- Fatty-acid metabolism disorders
- Autosomal recessive disorders
Wikimedia Foundation. 2010.