- Fibrocystic breast changes
-
Fibrocystic breast changes Classification and external resources 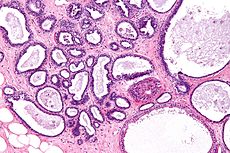
Micrograph showing fibrocystic breast changes. H&E stain.ICD-10 N60.1 ICD-9 610.1 DiseasesDB 4799 MedlinePlus 000912 MeSH D005348 Fibrocystic breast changes or fibrocystic breast disease is a condition of breast tissue affecting an estimated 30-60% of women. It is characterized by noncancerous breast lumps in the breast which can sometimes cause discomfort, often periodically related to hormonal influences from the menstrual cycle.
Contents
Terminology
In ICD-10 the condition is called diffuse cystic mastopathy, or, if there is epithelial proliferation, fibrosclerosis of breast.[1] Older names for this condition include chronic cystic mastitis, fibrocystic mastopathy and mammary dysplasia. The condition has also been named after several people (see eponyms below). Since it is a very common disorder, some authors have argued that it should not be termed a "disease",[2] whereas others feel that it meets the criteria for a disease. It is not a classic form of mastitis (breast inflammation).
Symptoms
The changes in fibrocystic breast disease are characterised by the appearance of fibrous tissue and a lumpy, cobblestone texture in the breasts. These lumps are smooth with defined edges, and are usually free-moving in regard to adjacent structures. The bumps can sometimes be obscured by irregularities in the breast that are associated with the condition. The lumps are most often found in the upper, outer sections of the breast (nearest to the armpit). Women with fibrocystic changes may experience a persistent or intermittent breast aching or breast tenderness related to periodic swelling. Breasts and nipples may be tender or itchy.
Symptoms follow a periodic trend tied closely to the menstrual cycle. Symptoms tend to peak immediately before each period and decrease afterwards. At peak, breasts may feel full and swollen. No complications related to breastfeeding have been found.
Causes
The causes of the condition are not fully understood, though it is known that they are tied to hormone levels, as the condition usually subsides after menopause and is also related to the menstrual cycle.
Fibrocystic breast changes is a cumulative process, caused partly by the normal hormonal variation during a woman's monthly cycle. The most important of these hormones are estrogen, progesterone and prolactin.
These hormones directly affect the breast tissues by causing cells to grow and multiply.[3] Many other hormones such as TSH, insulin, growth hormone and growth factors such as TGF-beta exert direct and indirect effects amplifying or regulating cell growth. Years of such fluctuations eventually produce small cysts and/or areas of dense or fibrotic tissue. Multiple small cysts and an increasing level of breast pain commonly develop when a woman hits her 30s. Larger cysts usually do not occur until after the age of 35.[4] Over time, presumably driven by aberrant growth signals, such lesions may accumulate epigenetic, genetic and karyotypic changes such as modified expression of hormone receptors and loss of heterozygosity.
Several variants of fibrocystic breast changes may be distinguished and these may have different causes and genetic predispostions. Adenosis involves abnormal count and density of lobular units, while other lesions appear to stem mainly from ductal epithelial origins.
Diagnosis
Diagnosis is mostly done based on symptoms after exclusion of breast cancer. Nipple fluid aspiration can be used to classify cyst type (and to some extent improve breast cancer risk prediction) but it is rarely used in practice. Biopsy or fine needle aspiration are rarely warranted.
Tests
Fibrocystic breast disease is primarily diagnosed based on the symptoms, clinical breast exam and on a physical exam. During this examination, the doctor checks for unusual areas in the breasts, both visually and manually. Also, the lymph nodes in the axilla area and lower neck are examined. A complete and accurate medical history is also helpful in diagnosing this condition. If the patient's medical history and physical exam findings are consistent with normal breast changes, no additional tests are considered but otherwise the patient will be asked to return a few weeks later for reassessment.[5] Women may detect lumps in their breasts during self-examination as well.
In order to establish whether the lump is a cyst or not, several imagining tests may be performed. Mammography is usually the first imaging test to be ordered when unusual breast changes have been detected during a physical examination. A diagnostic mammography consists in a series of x-rays that provide clear images of specific areas of the breast. Mammographies are recommended in women over 30 years old even though there are no suspicious findings during the physical examination.
Ultrasounds are commonly performed in conjunction with mammographies as they produce clear images of the breast and clearly distinguish between fluid-filled breast cysts and solid masses. The ultrasound exam can better evaluate dense tissue of the breast; hence it is often undergone by young patients, under 30 years old.
The breast biopsy is usually the test used to confirm the suspected diagnosing. After imaging tests have been performed and have revealed unusual areas or lumps in the breast, a breast biopsy will be ordered. This test consists in removing a sample of breast tissue which is then looked at under a microscope. The specialist analyzing the tissue sample will be able to conclude if the breast changes are benign or malignant or whether breast fibrocystic disease is present.
There are four main types of breast biopsies that may be performed. A fine-needle aspiration biopsy is usually ordered when the doctor is almost certain that the lump is a cyst.[6] This test is generally performed in conjunction with an ultrasound which is helpful in guiding the needle into a small or hard to find lump. The procedure is painless and it consists in inserting a thin needle into the breast tissue while the lump is palpated.
The core-needle biopsy is normally performed under local anesthesia and in a physician's office. The needle used in this procedure is slightly larger than the one used for a fine-needle biopsy because the procedure is intended to remove a small cylinder of tissue that will be sent to the laboratory for further examination.
A newer type of breast biopsy is the stereotactic biopsy that relies on a three-dimensional x-ray to guide the needle biopsy of non-palpable mass. The biopsy is performed in a similar matter, by using a needle to remove tissue sample but locating the specific area of the breast is done by x-raying the breast by two different angles.
Surgical biopsy is a procedure performed to remove the entire lump or a part of it for laboratory analyzing. It may be painful and it is done under local anesthesia.
Treatment
Most women with fibrocystic changes and no symptoms do not need treatment, but closer follow-up may be advised.[7]
There is no widely accepted treatment or prevention strategy for fibrocystic condition. When treatment of symptoms is necessary it follows the same strategies as treatment for cyclical breast pain.
Main article: Mastodynia#Treatments for cyclical breast painOnly a very small number of cysts are aspirated.
Prognosis
There are usually no adverse side effects to this condition. In almost all cases it subsides after menopause. A possible complication arises through the fact that cancerous tumors may be more difficult to detect in women with fibrocystic changes.
Breast cancer risk
Breast cancer risk is elevated for small fraction of lesions. Nonproliferative lesions have no increased risk, proliferative lesions approximately 2-fold risk. Atypical lobular hyperplasia is associated with the greatest risk, approximately 5-fold and especially high relative risk of developing premenopausal breast cancer. Atypical ductal hyperplasia is associated with 2.4-fold risk. [8]
It is not well understood whether the lesions are precursors of breast cancer or only indication of increased risk, for most types of lesions the chance of developing breast cancer is nearly the same in the affected and unaffected breast (side) indicating only coincidence of risk factors. For atypical lobular hyperplasia there is high incidence of ipsilateral breast cancers indicating a possible direct carcinogenetic link. [9]
Eponyms
This entity has historically also been termed Bloodgood’s disease, Cooper's disease (after Sir Astley Paston Cooper, 1st baronet), Phocas' disease, Reclus’ disease and Reclus’ syndrome (after Paul Reclus), Reclus-Schimmelbusch disease, Schimmelbusch disease and Tillaux-Phocas disease.[10]
See also
Additional images
-
Micrograph showing apocrine metaplasia associated with FCC. FNA specimen. Pap stain.
References
- ^ Disorders of breast (N60-N64) in ICD-10.
- ^ Santen RJ, Mansel R (July 2005). "Benign breast disorders". N. Engl. J. Med. 353 (3): 275–85. doi:10.1056/NEJMra035692. PMID 16034013.
- ^ "Fibrocystic Breast Condition". http://www.medicinenet.com/fibrocystic_breast_condition/page2.htm#13whatcauses.2010/04/13
- ^ "Fibrocystic Breast Condition". http://www.healthscout.com/ency/68/167/main.html#CausesandRiskFactorsofFibrocysticBreastDisease.2010/04/13
- ^ "Tests and diagnosis". http://www.mayoclinic.com/health/fibrocystic-breasts/DS01070/DSECTION=tests-and-diagnosis.2010/04/13
- ^ "Diagnosing Fibrocystic Breast Disease". http://www.lef.org/protocols/prtcl-145a.shtml#diag.2010/04/13
- ^ "Types of non-cancerous breast conditions". http://www.cancer.org/docroot/CRI/content/CRI_2_6X_Non_Cancerous_Breast_Conditions_59.asp#Types_of_non-cancerous_breast_conditions.2010/04/13
- ^ Marshall, LM; Hunter, DJ; Connolly, JL; Schnitt, SJ; Byrne, C; London, SJ; Colditz, GA (1997). "Risk of breast cancer associated with atypical hyperplasia of lobular and ductal types". Cancer Epidemiology, Biomarkers & Prevention 6 (5): 297–301. PMID 9149887.
- ^ Page, D. L.; Schuyler, P. A.; Dupont, W. D.; Jensen, R. A.; Plummer Jr, W. D.; Simpson, J. F. (2003). "Atypical lobular hyperplasia as a unilateral predictor of breast cancer risk: a retrospective cohort study". The Lancet 361: 125. doi:10.1016/S0140-6736(03)12230-1. PMID 12531579.
- ^ synd/1891 at Who Named It?
Disorders of breast (N60–N64, 610–611) Mastitis Puerperal mastitis (Breast engorgement) · Nonpuerperal mastitis (Subareolar abscess/Zuska's disease, Granulomatous mastitis)Other Benign mammary dysplasia (Duct ectasia of breast · Chronic cystic mastitis) · Galactorrhea · Mastodynia · nipple (Nipple discharge, Inverted nipple, Fissure of the nipple) · Galactocele · Ptosis · Breast cyst · Breast lump · Fat necrosis of breast · Gynecomastia · Hypertrophy of breastCategories:- Breast diseases
-
Wikimedia Foundation. 2010.

