- Marasmus
-
Marasmus Classification and external resources 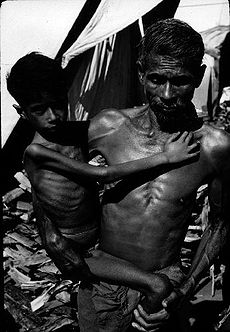
Child suffering with Marasmus in IndiaICD-10 E41.-E42. ICD-9 261 DiseasesDB 7826 eMedicine ped/164 MeSH D011502 Marasmus is a form of severe protein-energy malnutrition characterized by energy deficiency.
A child with marasmus looks emaciated. Body weight may be reduced to less than 80% of the average weight that corresponds to the height .[citation needed] Marasmus occurrence increases prior to age 1, whereas kwashiorkor occurrence increases after 18 months. It can be distinguished from kwashiorkor in that kwashiorkor is protein wasting with the presence of edema.
The prognosis is better than it is for kwashiorkor.[1]
The word “marasmus” comes from the Greek μαρασμός marasmos "consumption" from μαραίνειν marainein "to consume, exhaust."
Contents
Signs and symptoms
The malnutrition associated with marasmus leads to extensive tissue and muscle wasting, as well as variable edema. Other common characteristics include dry skin, loose skin folds hanging over the buttocks (glutei) and armpit (axillae), etc. There is also drastic loss of adipose tissue (body fat) from normal areas of fat deposits like buttocks and thighs. The afflicted are often fretful, irritable, and voraciously hungry.
Marasmus is generally known as the gradual wasting away of the body due to severe malnutrition or inadequate absorption of food. Marasmus is a form of severe protein deficiency and is one of the forms of protein-energy malfunction (PEM). It is a severe form of malnutrition caused by inadequate intake of proteins and calories.
Causes
Marasmus is caused by a severe deficiency of nearly all nutrients, especially protein and carbohydrates.
Treatment
It is necessary to treat not only the symptoms but also the complications of the disorder, including infections, dehydration, and circulation disorders, which are frequently lethal and lead to high mortality if ignored.
Ultimately, marasmus can progress to the point of no return when the body's machinery for protein synthesis, itself made of protein, has been degraded to the point that it cannot handle any protein. At this point, attempts to correct the disorder by giving food or protein are futile.
Epidemiology
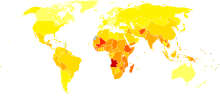 Disability-adjusted life year for protein-energy malnutrition per 100,000 inhabitants in 2002.[2]
Disability-adjusted life year for protein-energy malnutrition per 100,000 inhabitants in 2002.[2] no dataless than 1010-100100-200200-300300-400400-500500-600600-700700-800800-10001000-1350more than 1350
no dataless than 1010-100100-200200-300300-400400-500500-600600-700700-800800-10001000-1350more than 1350See also
References
- ^ Badaloo AV, Forrester T, Reid M, Jahoor F (June 2006). "Lipid kinetic differences between children with kwashiorkor and those with marasmus". Am. J. Clin. Nutr. 83 (6): 1283–8. PMID 16762938. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=16762938.
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002. http://www.who.int/entity/healthinfo/statistics/bodgbddeathdalyestimates.xls.
Nutrition disorders (E40–E68, 260–269) Hypoalimentation/
malnutritionB1: Beriberi/Wernicke's encephalopathy (Thiamine deficiency) · B2: Ariboflavinosis · B3: Pellagra (Niacin deficiency) · B6: Pyridoxine deficiency · B7: Biotin deficiency · B9: Folate deficiency · B12: Vitamn B12 deficiencyA: Vitamin A deficiency/Bitot's spots · C: Scurvy · D: Hypovitaminosis D/Rickets/Osteomalacia · E: Vitamin E deficiency · K: Vitamin K deficiencyHyperalimentation Mineral overloadM: NUT
cof, enz, met
noco, nuvi, sysi/epon, met
drug(A8/11/12)
Categories:
Wikimedia Foundation. 2010.
