- Optical window in biological tissue
-
The Optical window [1] (also known as therapeutic window) defines the range of wavelengths where light has its maximum depth of penetration in tissue. Within the NIR window, scattering is the most dominant light-tissue interaction, and therefore the propagating light becomes diffuse rapidly. Since scattering increases the distance travelled by photons within tissue, the probability of photon absorption also increases. Because scattering has weak dependence on wavelength, the optical window is primarily limited by absorption, due to either blood at short wavelengths or water at long wavelengths.Contents
Absorption properties of tissue components
The absorption coefficient (
 ) is defined as the probability of photon absorption in tissue per unit path length [2]. Different tissue components have different
) is defined as the probability of photon absorption in tissue per unit path length [2]. Different tissue components have different  values. Moreover,
values. Moreover,  is a function of wavelength. Below are discussed the absorption properties of the most important chromophores in tissue. Also, molar extinction coefficient (
is a function of wavelength. Below are discussed the absorption properties of the most important chromophores in tissue. Also, molar extinction coefficient ( ) is another parameter that is often used to describe photon absorption in tissue. By multiplying e by the molar concentration and by ln(10), one can convert
) is another parameter that is often used to describe photon absorption in tissue. By multiplying e by the molar concentration and by ln(10), one can convert  to
to  .
.
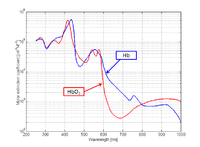
Blood: Blood consists of two different types of hemoglobin: oxyhemoglobin ( ) is bound to oxygen, while deoxyhemoglobin (
) is bound to oxygen, while deoxyhemoglobin ( ) is unbound to oxygen. These two different types of hemoglobin exhibit different absorption spectra that are normally represented in terms of molar extinction coefficients, as shown in Figure 1. The molar extinction coefficient of Hb has its highest absorption peak at 420 nm and a second peak at 580 nm. Its spectrum then gradually decreases as light wavelength increases. On the other hand,
) is unbound to oxygen. These two different types of hemoglobin exhibit different absorption spectra that are normally represented in terms of molar extinction coefficients, as shown in Figure 1. The molar extinction coefficient of Hb has its highest absorption peak at 420 nm and a second peak at 580 nm. Its spectrum then gradually decreases as light wavelength increases. On the other hand,  shows its highest absorption peak at 410 nm, and two secondary peaks at 550 nm and 600 nm. As light wavelengths passes 600 nm,
shows its highest absorption peak at 410 nm, and two secondary peaks at 550 nm and 600 nm. As light wavelengths passes 600 nm,  absorption decays much faster than Hb absorption. The points where the molar extinction coefficient spectra of
absorption decays much faster than Hb absorption. The points where the molar extinction coefficient spectra of  and
and  intersect are called isosbestic points.
intersect are called isosbestic points.
By using two different wavelengths, it is possible to calculate the concentrations of oxyhemoglobin ( ) and deoxyhemoglobin (
) and deoxyhemoglobin ( ) as shown in the following equations:
) as shown in the following equations:Here,
 and
and  are the two wavelengths;
are the two wavelengths;  and
and  are the molar extinction coefficients of
are the molar extinction coefficients of  and
and  , respectively;
, respectively;  and
and  are the molar concentrations of
are the molar concentrations of  and
and  in tissue, respectively. Oxygen saturation (
in tissue, respectively. Oxygen saturation ( ) can then be computed as
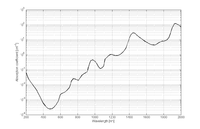
) can then be computed asWater: Although water is nearly transparent in the range of visible light, it becomes absorbing over the near-infrared region. Water is a critical component since its concentration is high in human tissue. The absorption spectrum of water in the range from 250 to 1000 nm is shown in Figure 2.
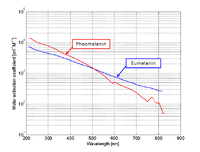
Other tissue components with less significant contributions to the total absorption spectrum of tissue are melanin and fat.Melanin: Melanin is a chromophore that exists in the human epidermal layer of skin responsible for protection from harmful UV radiation. When melanocytes are stimulated by solar radiation, melanin is produced[6]. Melanin is one of the major absorbers of light in some biological tissue (although its contribution is smaller than other components). There are two types of melanin: eumelanin which is black-brown and pheomelanin which is red-yellow[7]. The molar extinction coefficient spectra corresponding to both types are shown in Figure 3.
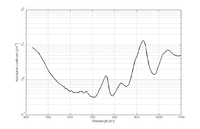
Fat: Fat is one of the major components in tissue that can comprise 10-40% of tissue. Although not many mammalian fat spectra are available, Figure 4 shows an example extracted from [8]. This plot was obtained from clear purified oil from pig lard. The detailed purification process is explained in [8].Scattering properties of tissue components
Optical scattering occurs due to mismatches in refractive index of the different tissue components, ranging from cell membranes to whole cells. Cell nuclei and mitochondria are the most important scatterers [2]. Their dimensions range from 100 nm to 6 μm. Most of these organelles exhibit highly forward-directed scattering [6].
Light scattering in biological tissue is denoted by the scattering coefficient (μs), which is defined as the probability of photon scattering in tissue per unit path length [2].Effective attenuation coefficient
Attenuation of light in deep biological tissue depends on the effective attenuation coefficient ( ), which is defined as
), which is defined as
where is the transport scattering coefficient defined as
is the transport scattering coefficient defined aswhere g is the anisotropy of biological tissue, which has a representative value of 0.9. Figure 5 shows a plot of transport scattering coefficient spectrum in breast tissue, which has a wavelength dependence of
 [9]. The effective attenuation coefficient is the dominant factor for determining light attenuation at depth
[9]. The effective attenuation coefficient is the dominant factor for determining light attenuation at depth  >> 1/
>> 1/  .
.Estimation of the optical window in tissue
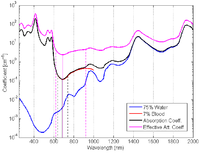
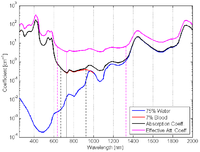
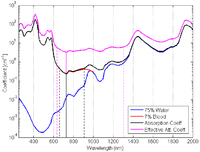
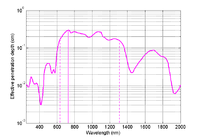
The optical window can be computed based on the absorption coefficient spectrum or the effective attenuation coefficient spectrum. A possible criterion for selecting the NIR window is given by the FWHM of the inverse of these spectra as shown in Figure 7.
In addition to the total concentration of hemoglobin, the oxygen saturation will define the concentration of oxy and deoxyhemoglobin in tissue and so the total absorption spectrum. Depending on the type of tissue, we can consider different situations.Below, the total concentration of hemoglobin is assumed to be 2.3 mM.
Figure 6 (a): Spectra for arteries (SaO2 ≈ 98%).Absorption coefficient: λmin = 686 nm; NIR window = (634 - 756) nm.
Effective attenuation coefficient: λmin = 690 nm; NIR window = (618 - 926) nm.
Figure 6 (b): Spectra for veins (SvO2 ≈ 60%).Absorption coefficient: λmin = 730 nm; NIR window = (664 - 932) nm.
Effective attenuation coefficient: λmin = 730 nm; NIR window = (630 - 1328) nm.
Absorption spectrum for arteries: In this case
 ≈ 98% (arterial oxygen saturation). Then oxyhemoglobin will be dominant in the total absorption (black) and the effective attenuation (magenta) coefficient spectra, as shown in Figure 6 (a).
≈ 98% (arterial oxygen saturation). Then oxyhemoglobin will be dominant in the total absorption (black) and the effective attenuation (magenta) coefficient spectra, as shown in Figure 6 (a).
Absorption spectrum for veins: In this case ≈ 60% (venous oxygen saturation). Then oxyhemoglobin and deoxyhemoglobin will have similar contributions to the total absorption (black) and the effective attenuation (magenta) coefficient spectra, as shown in Figure 6 (b).
≈ 60% (venous oxygen saturation). Then oxyhemoglobin and deoxyhemoglobin will have similar contributions to the total absorption (black) and the effective attenuation (magenta) coefficient spectra, as shown in Figure 6 (b).Absorption spectrum for breast tissue: To define
 (tissue oxygen saturation) it is necessary to define a distribution of arteries and veins in tissue. an arterial-venous blood volume ratio of 20%/80% can be adopted [10]. Thus tissue oxygen saturation can be defined as
(tissue oxygen saturation) it is necessary to define a distribution of arteries and veins in tissue. an arterial-venous blood volume ratio of 20%/80% can be adopted [10]. Thus tissue oxygen saturation can be defined as  = 0.2 x
= 0.2 x  + 0.8 x
+ 0.8 x  ≈ 70%.
≈ 70%.The total absorption (black) and the effective attenuation (magenta) coefficient spectra for breast tissue is shown in Figure 6 (c).In addition, the effective penetration depth is plotted in Figure 7.
See also
References
- ^ Tromberg, B.J., Shah, N., Lanning, R., Cerussi, A., Espinoza, J., Pham, T., Svaasand, L., and Butler, J. (2000). Non-invasive in vivo characterization of breast tumors using photon migration spectroscopy. Neoplasia 2, 26–40
- ^ a b c LV Wang and HI Wu (2007). Biomedical Optics. Wiley. ISBN 9780471743040.
- ^ Molar extinction coefficients of oxy and deoxyhemoglobin compiled by Scott Prahl. URL: http://omlc.ogi.edu/spectra/hemoglobin.
- ^ G. M. Hale, and M. R. Querry, Optical constants of water in the 200 nm to 200 µm wavelength region, Appl. Opt., 12, 555-563, 1973.
- ^ S. Jacques, Extinction coefficient of melanin. URL: http://omlc.ogi.edu/spectra/melanin/extcoeff.html.
- ^ a b T. Vo-Dinh (2002). Biomedical Photonics Handbook. Taylor & Francis, Inc.. ISBN 0849311160.
- ^ George Zonios and Aikaterini Dimou, Ioannis Bassukas, Dimitrios Galaris, and Argyrios Ysolakidis and Efthimios Kaxiras, J. Biomed. Opt., Vol.13, 014017, 2008.
- ^ a b c R.L.P. van Veen, H.J.C.M. Sterenborg, A. Pifferi, A. Torricelli, and R. Cubeddu, OSA Annual BIOMED Topical Meeting, 2004
- ^ a b S. Srinivasan, B. Pogue, S. Jiang, H. Dehghani, C. Kogel, S. Soho, J. Gibson, T. Tosteson, S. Poplack, and K. Paulsen, K D 2003, Proc Natl Acad. Sci. USA 100 12349 54.
- ^ S. Nioka, S. Wen, J. Zhang, J. Du, X. Intes, Z. Zhao, and B. Chance, Simulation study of breast tissue hemodynamics during pressure perturbation. Oxygen Transport to Tissue XXVI 566, 17-22, 2006.
Categories:- Infrared imaging
- Biophysics
Wikimedia Foundation. 2010.