- Medicare fraud
-
In the United States, Medicare fraud is a general term that refers to an individual or corporation that seeks to collect Medicare health care reimbursement under false pretenses. There are many different types of Medicare fraud, all of which have the same goal: to collect money from the Medicare program illegitimately.
The total amount of Medicare fraud is difficult to track, because not all fraud is detected and not all suspicious claims turn out to be fraudulent. According to the Office of Management and Budget, Medicare "improper payments" were $47.9 billion in 2010, but some of these payments later turned out to be valid.[1] The Congressional Budget Office estimates that total Medicare spending was $528 billion in 2010.[2]
The Medicare program is a target for fraud because it is based on the "honor system" of billing. It was originally set-up to help honest doctors who helped the needy with medical services. There are few safeguards to eliminate false claims.[citation needed] In fact, claims are paid automatically because the goal of Medicare is not to root out false claims, but to pay claims quickly and smoothly.
Contents
Types of Medicare fraud
Medicare fraud is typically seen in the following ways:[3][specify]
- Phantom Billing: The medical provider bills Medicare for unnecessary procedures, or procedures that are never performed; for unnecessary medical tests or tests never performed; for unnecessary equipment; or equipment that is billed as new but is, in fact, used. In which case, every form of billing, phantom or patient, can be prevented through carefully checking.
- Patient Billing: A patient who is in on the scam provides his or her Medicare number in exchange for kickbacks. The provider bills Medicare for any reason and the patient is told to admit that he or she indeed received the medical treatment.
- Upcoding scheme and unbundling: Inflating bills by using a billing code that indicates the patient needs expensive procedures.
A 2011 crackdown on fraud charged "111 defendants in nine cities, including doctors, nurses, health care company owners and executives" of fraud schemes involving "various medical treatments and services such as home health care, physical and occupational therapy, nerve conduction tests and durable medical equipment."[4]
In recent years, as regulatory requirements tightened[5] and law enforcement has stepped up, Medicare fraud has shifted away from sectors such as durable medical equipment[6] and HIV/AIDS infusion injections and into other areas such as ambulance fraud and hospice care fraud.[7][8] Durable medical equipment or home medical equipment describes medically required equipment and services used in the home such as wheelchairs, hospital beds, nebulizers, and oxygen equipment, and represents less than two percent of total Medicare spending.[9]
Even in other countries, particularly in South-East Asia, there are doctors who over-charge American patients, through Medicare (or Tricare), charging them US rates, much higher than actual medical cost in their respective countries. This is a type of insurance fraud, which, unfortunately, Medicare continually overlooks and fails to take into account.[citation needed]
Prime Healthcare
Prime Healthcare Services is under investigation by the United States Department of Health and Human Services and the California Department of Justice about concerns over a reported spike in septicemia. The investigation centers around whether the spike in septicemia represents a large public health issue or multimillion-dollar Medicare fraud. Six Prime hospitals ranked in the 99th percentile of U.S. hospitals for septicemia and five were in the 95th percentile.[10]
There is also evidence that Prime Healthcare Service engages in upcoding elderly patients to malnutrition. In Mount Shasta, Victorville and in the Mojave Desert, Prime has had high rates of kwashiorkor amongst its elderly patients. At Shasta Regional Medical Center, Prime reported 16.1% of their Medicare patients suffered from kwashiorkor. The state of California average for Medicare patients is 0.2% suffering from kwashiorkor.[11]
Prime also has come under scrutiny by investigators over expenses on luxury items disallowed by Medicare. Authorities have flagged $491,000 in operating costs in relation to a Eurocopter for the Chief Executive Officer, Lex Reddy. The Department of Health Care Services also identified and disallowed $820,000 for the lease and taxes on a home in Beverly Hills and $303,000 in depreciation on the Helicopter and a Bentley. The funds flagged by auditors do not represent tax dollars that have been sent to Prime. Rather, they signify sums that the state will not recognize when compensating the chain for its corporate office expenses.[11]
Prime maintains that their billing practices are legal and proper and claim that the high rate of kwashiorkor is a result of proper diagnosis of malnutrition. They also claim that they are the victim of a campaign by SEIU, but the California Medi-Cal fraud director has stated that his bureau had initiated an investigation before SEIU released their findings.[11]
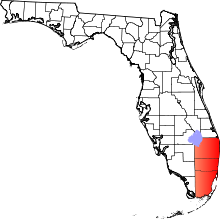
South Florida
The South Florida area has become the epicenter of Medicare fraud in the United States. In 2008, criminals from two Florida counties alone accounted for approximately $400 million in fraudulent Medicare bills.[citation needed] Also in 2008, Miami-Dade County billed Medicare six times more for home health services than Los Angeles County, where the Medicare population is three times larger.[citation needed] In fact, the problem has become so rampant that in 2008, federal investigators found nearly half of all DME suppliers in South Florida were not in compliance with Medicare rules. In response, the authorities required every single medical equipment supplier to re-apply for billing privileges.[12]
In 2005, 72% of all Medicare claims nationwide for HIV/AIDS infusion injections were billed in Miami-Dade County.[citation needed] Many recent immigrants to South Florida open up a company and immediately start billing Medicare for tens of thousands in equipment and services that Medicare beneficiaries never receive.[citation needed]
Many South Florida drug dealers look to Medicare fraud as the new crime of choice. Criminals, now federal defendants, report that (1) there is more money in Medicare fraud than in drug smuggling, (2) there is a lesser chance of being caught and, (3) if caught, defendants are treated like a white collar criminal as opposed to a drug dealer.[citation needed]
Columbia/HCA fraud case
The Columbia/HCA fraud case is one of the largest examples of Medicare fraud in U.S. history. Numerous New York Times stories, beginning in 1996, began scrutinizing Columbia/HCA's business and Medicare billing practices. These culminated in the company being raided by Federal agents searching for documents and eventually the ousting of the corporation's CEO, Rick Scott, by the board of directors.[13] Among the crimes uncovered were doctors being offered financial incentives to bring in patients, falsifying diagnostic codes to increase reimbursements from Medicare and other government programs, and billing the government for unnecessary lab tests,[14] though Scott personally was never charged with any wrongdoing. HCA wound up pleading guilty to more than a dozen criminal and civil charges and paying fines totaling $1.7 billion. In 1999, Columbia/HCA changed its name back to HCA, Inc.
In 2001, HCA reached a plea agreement with the U.S. government that avoided criminal charges against the company and included $95 million in fines.[15] In late 2002, HCA agreed to pay the U.S. government $631 million, plus interest, and pay $17.5 million to state Medicaid agencies, in addition to $250 million paid up to that point to resolve outstanding Medicare expense claims.[16] In all, civil law suits cost HCA more than $1.7 billion to settle, including more than $500 million paid in 2003 to two whistleblowers.[15]
Law enforcement and prosecution
The Office of Inspector General for the U.S. Department of Health and Human Services, as mandated by Public Law 95-452 (as amended), is to protect the integrity of Department of Health and Human Services (HHS) programs, to include Medicare and Medicaid programs, as well as the health and welfare of the beneficiaries of those programs. The Office of Investigations for the HHS, OIG collaboratively works with the Federal Bureau of Investigation in order to combat Medicare Fraud.
Defendants convicted of Medicare fraud face stiff penalties according to the Federal Sentencing Guidelines and disbarment from HHS programs. The sentence depends on the amount of the fraud. Defendants can expect to face substantial prison time, deportation (if not a US citizen), fines, and restitution.
In 1997, the federal government dedicated $100 million to federal law enforcement to combat Medicare fraud. That money pays over 400 FBI agents who investigate Medicare fraud claims. In 2007, the U.S. Department of Health and Human Services, Office of Inspector General, U.S. Attorney's Office, and the U.S. Department of Justice created the Medicare Fraud Strike Force in Miami, Florida.[12] This group of anti-fraud agents has been duplicated in other cities where Medicare fraud is widespread. In Miami alone, over two dozen agents from various federal agencies investigate solely Medicare fraud. In May 2009, Attorney General Holder and HHS Secretary Sebelius Announce New Interagency Health Care Fraud Prevention and Enforcement Action Team (HEAT) to combat Medicare fraud.[17] FBI Director Robert Mueller stated that the FBI and HHS OIG has over 2,400 open health care fraud investigations.[18]
The first "National Summit on Health Care Fraud” was held on January 28, 2010 to bring together leaders from the public and private sectors to identify and discuss innovative ways to eliminate fraud, waste and abuse in the U.S. health care system.[19] The summit is the first national gathering on health care fraud between law enforcement and the private and public sectors and is part of the Obama Administration’s coordinated effort to fight health care fraud.
2010 Medicare Fraud Strike Task Force Charges
In July 2010, the Medicare Fraud Strike Task Force announced its largest fraud discovery ever when charging 94 people nationwide for allegedly submitting a total of $251 million in fraudulent Medicare claims. The 94 people charged included doctors, medical assistants, and health care firm owners, and 36 of them have been found and arrested.[20][21] Charges were filed in Baton Rouge (31 defendants charged), Miami (24 charged) Brooklyn, (21 charged), Detroit (11 charged) and Houston (four charged).[20] By value, nearly half of the false claims were made in Miami-Dade County, Florida.[21] The Medicare claims covered HIV treatment, medical equipment, physical therapy and other unnecessary services or items, or those not provided.[22]
2011 Medicare Fraud Strike Task Force Charges
In Septemer 2011, a nationwide takedown by Medicare Fraud Strike Force operations in eight cities resulted in charges against 91 defendants for their alleged participation in Medicare fraud schemes involving approximately $295 million in false billing.[23]
Organized crime
Main article: 2010 Medicaid FraudMedicare has been defrauded in a larger medical scam involving a criminal ring's attempt to steal $163 million dollars from various healthcare organizations. Of the 73 individuals indicted for this scheme, more than 50 people were arrested on October 13, 2010 in New York, California, New Mexico, Ohio and Georgia.[24][25]
See also
References
- ^ politifact.com (2011-01-04). Retrieved on 2011-01-05.
- ^ "The Budget and Economic Outlook: Fiscal Years 2010 to 2020". Congressional Budget Office. http://www.cbo.gov/ftpdocs/108xx/doc10871/01-26-Outlook.pdf.
- ^ medicare.gov
- ^ hhs.gov
- ^ cms.gov
- ^ oig.hhs.gov
- ^ m.npr.org
- ^ [1]
- ^ cms.gov
- ^ William, Lance; Christina Jewett (October 11, 2010). "Hospital chain’s high infection rate leads to fraudulent billing concerns". California Watch. http://californiawatch.org/health-and-welfare/hospital-chain-s-high-infection-rate-leads-fraudulent-billing-concerns-5647.
- ^ a b c Williams, Lance; Christina Jewett, Stephen K. Doig (February 19, 2011). "Hospital chain, already under scrutiny, reports high malnutrition rates". California Watch. http://californiawatch.org/health-and-welfare/hospital-chain-already-under-scrutiny-reports-high-malnutrition-rates-8786.
- ^ a b Feds Fight Rampant Medicare Fraud in South Florida. NPR. Retrieved on 2010-11-04.
- ^ Jacksonville Business Journal Friday, April 14, 2006
- ^ Bringing HCA Back to Life After years of scandal. Fortune Magazine Feb 2004
- ^ a b M.C. Moewe (April 14, 2006). "Ex-Columbia chief helps grow Solantic". Jacksonville Business Journal. http://www.bizjournals.com/jacksonville/stories/2006/04/17/story1.html.
- ^ Julie Appleby (December 18, 2002). "HCA to settle more allegations for $631M". USA Today. http://www.usatoday.com/money/industries/health/2002-12-18-hca-settlement-_x.htm.
- ^ Attorney General Holder and HHS Secretary Sebelius Announce New Interagency Health Care Fraud Prevention and Enforcement Action Team. Hhs.gov (2010-10-18). Retrieved on 2010-11-04.
- ^ Johnson, Carrie (June 25, 2009). "53 in Detroit and Miami Indicted in Medicare Fraud Sting". The Washington Post. http://www.washingtonpost.com/wp-dyn/content/article/2009/06/24/AR2009062401906.html. Retrieved May 12, 2010.
- ^ Health & Human Services Secretary Kathleen Sebelius, Attorney General Eric Holder Convene National Summit on Health Care Fraud, Unveil Historic Commitment to Fighting Fraud in President’s FY 2011 Budget. Hhs.gov (2010-10-18). Retrieved on 2010-11-04.
- ^ a b Federal Bureau of Investigation press release, July 16, 2010, Medicare Fraud Strike Force Charges 94 Doctors, Health Care Company Owners, Executives, and Others for More Than $251 Million in Alleged False Billing
- ^ a b Miami Herald, Feds charge 94 medicare suspects in Miami other cities, July 17, 2010, Jay Weaver
- ^ Authorities charge 94 suspects for medicare fraud, PBS Newshour, July 16, 2010, accessed July 17, 2010, Lea Winerman
- ^ "Medicare Fraud Strike Force Charges 91 Individuals for Approximately $295 Million in False Billing" (Press release). U.S. Department of Justice. September 07, 2011. http://www.fbi.gov/news/pressrel/press-releases/medicare-fraud-strike-force-charges-91-individuals-for-approximately-295-million-in-false-billing. Retrieved September 10, 2011.
- ^ Ailsa Chang (October 14, 2010). "52 arrested in sweeping Medicare fraud case". National Public Radio. http://www.latimes.com/news/nationworld/nation/la-me-healthcare-fraud-raid-20101014,0,7387144.story. Retrieved October 18, 2010.
- ^ "Feds take down largest-ever Medicare fraud ring". Mass Device. October 14, 2010. http://www.massdevice.com/news/feds-take-down-largest-ever-medicare-fraud-ring. Retrieved October 18, 2010.
External links
- Stop Medicare Fraud site by US Government
- Fraud Overview at Medicare.gov site
- Medicare Fraud Reporting Center Information about Medicare fraud and how to report it.
Types of fraud Financial Advance-fee (Lottery scam) • Bank • Bankruptcy • Cheque • Credit card • Forex • Friendly • Insurance • Mortgage • Securities • TaxBusiness related Billing • Cramming • Disability • Drug/Pharmaceutical • Employment • Fixing • Identity theft • Intellectual property • Internet • Job • Long firm • Odometer • Phone • Quackery/Health care • Return • Slamming • TelemarketingFamily related Government related Other types Charity • Confidence trick • Counterfeiting • Forgery • Hoax • Identity theft • Mail and wire (honest services)Categories:- Health fraud
- Medicare and Medicaid (United States)
Wikimedia Foundation. 2010.