- Blastocystosis
DiseaseDisorder infobox
Name = Blastocystosis
Caption = "Blastocystis sp. "
DiseasesDB = 33233
ICD9 = ICD9|007|9
ICDO =
OMIM =
MeshID = D016776Blastocystosis refers to a medical condition caused by infection with "
Blastocystis ". "Blastocystis" is a highly prevalent single-celled parasite that infects the gastrointestinal tract of humans and animals. Many different types of "Blastocystis" exist, and they can infect humans, farm animals, birds, rodents, amphibians, reptiles, fish, and even cockroaches.cite journal |author=Yoshikawa H, Wu Z, Howe J, Hashimoto T, Geok-Choo N, Tan KS |title=Ultrastructural and phylogenetic studies on Blastocystis isolates from cockroaches |journal=J. Eukaryot. Microbiol. |volume=54 |issue=1 |pages=33–7 |year=2007 |pmid=17300516 |doi=10.1111/j.1550-7408.2006.00141.x] "Blastocystis" has presented a challenge to the medical and scientific community due to the diversity of hosts the organism can infect, the diversity of "Blastocystis" species which exist, and the fact that most species of "Blastocystis" found in mammals and birds are able to cause infection in humans. The organism has been called controversial, cryptic, and enigmatic. Even its classification has proved challenging. "Blastocystis" was originally classified as a yeast, then a protozoan. An analysis of its genetic content was performed in 1996, placing it into theStramenopile kingdom.cite journal |author=Silberman JD, Sogin ML, Leipe DD, Clark CG |title=Human parasite finds taxonomic home |journal=Nature |volume=380 |issue=6573 |pages=398 |year=1996 |pmid=8602239 |doi=10.1038/380398a0]For many years, scientists believed one species of "Blastocystis" infected humans, while other species of "Blastocystis" infected animals. So they called "Blastocystis" from humans "Blastocystis hominis" and named "Blastocystis" from other animals differently, for example "Blastocystis ratti" from rats. Genetic analysis performed in 2005 showed "Blastocystis hominis" does not really exist -- there is no unique species of "Blastocystis" that infects humans. cite journal |author=Noël C, Dufernez F, Gerbod D, "et al" |title=Molecular phylogenies of Blastocystis isolates from different hosts: implications for genetic diversity, identification of species, and zoonosis |journal=J. Clin. Microbiol. |volume=43 |issue=1 |pages=348–55 |year=2005 |pmid=15634993 |doi=10.1128/JCM.43.1.348-355.2005 ] In fact, nine different species groups of "Blastocystis" can infect humans, including "Blastocystis ratti." cite journal |author=Puthia MK, Sio SW, Lu J, Tan KS |title=Blastocystis ratti induces contact-independent apoptosis, F-actin rearrangement, and barrier function disruption in IEC-6 cells |journal=Infect. Immun. |volume=74 |issue=7 |pages=4114–23 |year=2006 |pmid=16790785 |doi=10.1128/IAI.00328-06 ] A tenth group was identified in China in 2007. cite journal |author=Li LH, Zhang XP, Lv S, "et al" |title=Cross-sectional surveys and subtype classification of human Blastocystis isolates from four epidemiological settings in China |journal= Parasitology Research|volume= 102|issue= |pages= 83|year=2007 |pmid=17912552 |doi=10.1007/s00436-007-0727-0] Because of this, in 2007 scientists proposed discontinuing the use of the term "Blastocystis hominis."cite journal |author=Stensvold CR, Suresh GK, Tan KS, "et al" |title=Terminology for Blastocystis subtypes--a consensus |journal=Trends Parasitol. |volume=23 |issue=3 |pages=93–6 |year=2007 |pmid=17241816 |doi=10.1016/j.pt.2007.01.004] Their proposal is to refer to "Blastocystis" from humans and animals according to the genetic identify of the "Blastocystis" organism, rather than the host that was infected by it.
Active Research Efforts
While many enteric protists are the subject of research, "Blastocystis" is unusual in that basic questions concerning how it should be diagnosed and treated and how it causes disease remain unsettled. The following groups have ongoing research programs directed at these questions:
Despite its prevalence, there is a lack of study regarding treatment of the infection. In-vitro antibiotic sensitivity testing is rarely reported. The following first-line treatments have been reported as successful in studies:
:
Metronidazole was reported as 100% successful in a 1991 study however in a subsequent study it was found to be less effective especially in patients classified as severely infected. cite journal |author=Moghaddam DD, Ghadirian E, Azami M |title=Blastocystis hominis and the evaluation of efficacy of metronidazole and trimethoprim/sulfamethoxazole |journal=Parasitol. Res. |volume=96 |issue=4 |pages=273–5 |year=2005 |pmid=15915364 |doi=10.1007/s00436-005-1363-1 ]:TMP-SMX was reported to slightly less effective than
Metronidazole in one study.:
Nitazoxanide was reported to be successful in a study authored by the drug's manufacturer. cite journal |author=Rossignol JF, Kabil SM, Said M, Samir H, Younis AM |title=Effect of nitazoxanide in persistent diarrhea and enteritis associated with Blastocystis hominis |journal=Clin. Gastroenterol. Hepatol. |volume=3 |issue=10 |pages=987–91 |year=2005 |pmid=16234044 |doi= ]:
Iodoquinol andParomomycin have been reported in the treatment of "Blastocystis" infection. cite journal |author=Armentia A, Méndez J, Gómez A, "et al" |title=Urticaria by Blastocystis hominis. Successful treatment with paromomycin |journal=Allergologia et immunopathologia |volume=21 |issue=4 |pages=149–51 |year=1993 |pmid=8237719 |doi= ]Iodoquinol has been found to be less effective in practice and in-vitro. cite journal |author=Grossman I, Weiss LM, Simon D, Tanowitz HB, Wittner M |title=Blastocystis hominis in hospital employees |journal=Am. J. Gastroenterol. |volume=87 |issue=6 |pages=729–32 |year=1992 |pmid=1590309 |doi= ] cite journal |author=Dunn LA, Boreham PF |title=The in-vitro activity of drugs against Blastocystis hominis |journal=J. Antimicrob. Chemother. |volume=27 |issue=4 |pages=507–16 |year=1991 |pmid=1856129 |doi= ]:
Miconazole has been reported as an agent against "Blastocystis" growth in-vitro. cite journal |author=Gonçalves AQ, Viana Jda C, Pires EM, Bóia MN, Coura JR, Silva EF |title=The use of the antifungal agent miconazole as an inhibitor of Blastocystis hominis growth in Entamoeba histolytica/E. dispar cultures |journal=Rev. Inst. Med. Trop. Sao Paulo |volume=49 |issue=3 |pages=201–2 |year=2007 |pmid=17625701 |doi= ]Treatment Failure: A 1916 report of "Blastocystis" infection described it as "an infection that is hard to get rid of", suggesting treatment failure may not be a recent phenomenon. A clinical report from 1986 identified cases that were non-responsive to several different antiprotozoal drugs. cite journal |author=Markell EK, Udkow MP |title=Blastocystis hominis: pathogen or fellow traveler? |journal=Am. J. Trop. Med. Hyg. |volume=35 |issue=5 |pages=1023–6 |year=1986 |pmid=3766850 |doi= ] An in-vitro study found 40% of isolates are resistant to common antiprotozoal drugs. cite journal |author=Haresh K, Suresh K, Khairul Anus A, Saminathan S |title=Isolate resistance of Blastocystis hominis to metronidazole |journal=Trop. Med. Int. Health |volume=4 |issue=4 |pages=274–7 |year=1999 |pmid=10357863 |doi= ] A study of isolates from patients diagnosed with IBS found 40% of isolates resistant to
Metronidazole and 32% resistant tofurazolidone . cite journal |author=Yakoob J, Jafri W, Jafri N, Islam M, Asim Beg M |title=In vitro susceptibility of Blastocystis hominis isolated from patients with irritable bowel syndrome |journal=Br. J. Biomed. Sci. |volume=61 |issue=2 |pages=75–7 |year=2004 |pmid=15250669 |doi= ] The problem of refractory cases is also described in a review article from anNIH lab and in a US report. cite book | last = Boorom | first = K | title = Commensal and Pathogenic Blastocystis with Case Studies from Oregon's Willamette Valley | Publisher = FBH Press | date=2006 | pages=112 | isbn=978-1430309048] Metronidazole resistance has been noted other protozoal infections, and compounds related to Metronidazole have been examined as alternative treatments. cite journal |author=Upcroft JA, Dunn LA, Wright JM, Benakli K, Upcroft P, Vanelle P |title=5-Nitroimidazole drugs effective against metronidazole-resistant Trichomonas vaginalis and Giardia duodenalis |journal=Antimicrob. Agents Chemother. |volume=50 |issue=1 |pages=344–7 |year=2006 |pmid=16377707 |doi=10.1128/AAC.50.1.344-347.2006]Discontinued and restricted treatments
Physicians have described the successful use of a variety of discontinued antiprotozoals in treatment of Blastocystis infection. The reduction in the availability of antiprotozoal drugs has been noted as a complicating factor in treatment of other protozoal infections. cite journal |author=White AC |title=The disappearing arsenal of antiparasitic drugs |journal=N. Engl. J. Med. |volume=343 |issue=17 |pages=1273–4 |year=2000 |pmid=11183360 |doi=] For example, in
Australia , production ofdiloxanide furoate ended in 2003,paromomycin is available under special access provisions, and the availability ofiodoquinol is limited. cite journal |author=van Hal SJ, Stark DJ, Fotedar R, Marriott D, Ellis JT, Harkness JL |title=Amoebiasis: current status in Australia |journal=Med. J. Aust. |volume=186 |issue=8 |pages=412–6 |year=2007 |pmid=17437396 |doi=] The following discontinued drugs have been reported as effective in treating Blastocystis infection::"
Emetine :" Use was reported as successful in cases in early 20th century with British soldiers who contracted "Blastocystis" infection while serving in Egypt. In-vitro testing showedemetine was more effective thanMetronidazole orfurazolidone . cite journal |author=Zierdt CH, Swan JC, Hosseini J |title=In vitro response of Blastocystis hominis to antiprotozoal drugs |journal=J. Protozool. |volume=30 |issue=2 |pages=332–4 |year=1983 |pmid=6631776 |doi=] Emetine is available in the United States only through special arrangement with theCenter for Disease Control .:"
Clioquinol (Entero-vioform):" AnNIH researcher noted that this drug was successful in treatment of "Blastocystis" infection but removed from the market following an adverse event in Japan.:"Stovarsol and Narsenol": These arsenic-based antiprotozoals were used extensively for treatment of bacterial and protozoal infections well into the 20th century. They have been reported to be effective against the infection. A third, Carbarsone, was available as an anti-infective compound in the United States as late as 1991, and was suggested as a possible treatment. They are no longer available for therapeutic use in humans, but other arsenic-based antiprotozoals remain in use for the treatment of "
Leishmania ."Diagnostic methods that are clinically available
Diagnosis is performed by determining if the infection is present, and then making a decision as to whether the infection is responsible for the symptoms. Diagnostic methods in clinical use have been reported to be of poor quality and more reliable methods have been reported in research papers. cite journal |author=Mahmoud MS, Saleh WA |title=Secretory and humoral antibody responses to Blastocystis hominis in symptomatic and asymptomatic human infections |journal=Journal of the Egyptian Society of Parasitology |volume=33 |issue=1 |pages=13–30 |year=2003 |pmid=12739797 |doi=] cite journal |author=Leelayoova S, Taamasri P, Rangsin R, Naaglor T, Thathaisong U, Mungthin M |title=In-vitro cultivation: a sensitive method for detecting Blastocystis hominis |journal=Ann. Trop. Med. Parasitol. |volume=96 |issue=8 |pages=803–7 |year=2002 |pmid=12625935 |doi=10.1179/000349802125002275] cite journal |author=Suresh K, Smith H |title=Comparison of methods for detecting Blastocystis hominis |journal=Eur. J. Clin. Microbiol. Infect. Dis. |volume=23 |issue=6 |pages=509–11 |year=2004 |pmid=15168139 |doi=10.1007/s10096-004-1123-7] cite journal |author=Stensvold R, Brillowska-Dabrowska A, Nielsen HV, Arendrup MC |title=Detection of Blastocystis hominis in unpreserved stool specimens by using polymerase chain reaction |journal=J. Parasitol. |volume=92 |issue=5 |pages=1081–7 |year=2006 |pmid=17152954 |doi=] cite journal |author=Parkar U, Traub RJ, Kumar S, "et al" |title=Direct characterization of Blastocystis from faeces by PCR and evidence of zoonotic potential |journal=Parasitology |volume=134 |issue=Pt 3 |pages=359–67 |year=2007 |pmid=17052374 |doi=10.1017/S0031182006001582 ]
For identification of infection, the only method clinically available in most areas is the "Ova and Parasite" (O&P) exam, which identifies the presence of the organism by microscopic examination of a chemically preserved stool specimen. This method is sometimes called "Direct Microscopy". In the United States, pathologists are required to report the presence of "Blastocystis" when found during an O&P exam, so a special test does not have to be ordered. Direct Microscopy is inexpensive, as the same test can identify a variety of gastrointestinal infections, such as
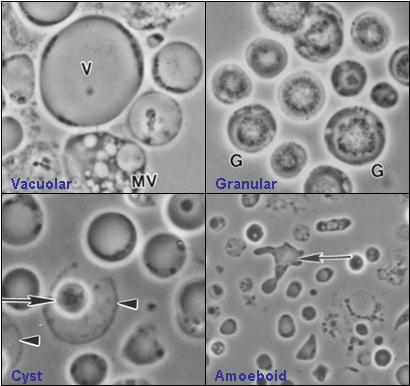
Giardia ,Entamoeba histolytica ,Cryptosporidium . However one laboratory director noted that pathologists using conventional microscopes failed to identify many "Blastocystis" infections, and indicated the necessity for special microscopic equipment for identification. The following table shows the sensitivity of Direct Microscopy in detecting "Blastocystis" when compared to stool culture, a more sensitive technique. Stool culture was considered by some researchers to be the most reliable technique, but a recent study found stool culture only detected 83% of individuals infected when compared topolymerase chain reaction (PCR) testing.Reasons given for the failure of Direct Microscopy include: (1) Variable Shedding: The quantity of "Blastocystis" organisms varies substantially from day to day in infected humans and animals; cite journal |author=Vennila GD, Suresh Kumar G, Khairul Anuar A, "et al" |title=Irregular shedding of Blastocystis hominis |journal=Parasitol. Res. |volume=85 |issue=2 |pages=162–4 |year=1999 |pmid=9934969 |doi=] (2) Appearance: Some forms of "Blastocystis" resemble fat cells or white blood cells , making it difficult to distinguish the organism from other cells in the stool sample; (3) Large number of morphological forms: "Blastocystis" cells can assume a variety of shapes, some have been described in detail only recently, so it is possible that additional forms exist but have not been identified.
Several methods have been cited in literature for determination of the significance of the finding of "Blastocystis":
#Diagnosis only when large numbers of organism present: Some physicians consider "Blastocystis" infection to be a cause of illness only when large numbers are found in stool samples. Researchers have questioned this approach, noting that it is not used with any other protozoal infections, such as
Giardia orEntamoeba histolytica . Some researchers have reported no correlation between number of organisms present in stool samples and the level of symptoms. A study usingpolymerase chain reaction testing of stool samples suggested that symptomatic infection can exist even when sufficient quantities of the organism do not exist for identification through Direct Microscopy.
#Diagnosis-by-exclusion: Some physicians diagnose "Blastocystis" infection by excluding all other causes, such as infection with other organisms, food intolerances, colon cancer, etc. This method can be time consuming and expensive, requiring many tests such asendoscopy andcolonoscopy .
#Disregarding "Blastocystis" : In the early to mid 1990s, some US physicians suggested all findings of "Blastocystis" are insignificant. No recent publications expressing this opinion could be found. cite journal |author=Markell EK |title=Is there any reason to continue treating Blastocystis infections? |journal=Clin. Infect. Dis. |volume=21 |issue=1 |pages=104–5 |year=1995 |pmid=7578717 |doi= ]Diagnostic methods that are not clinically available
The following diagnostic methods are not routinely available to patients. Researchers have reported that they are more reliable at detecting infection, and in some cases can provide the physician with information to help determine whether "Blastocystis" infection is the cause of the patient's symptoms:
Serum antibody testing: A 1993 research study performed by the
NIH with United States patients suggested that it was possible to distinguish symptomatic and asymptomatic infection with "Blastocystis" using serum antibody testing. cite journal |author=Zierdt CH, Nagy B |title=Antibody response to Blastocystis hominis infections |journal=Ann. Intern. Med. |volume=118 |issue=12 |pages=985–6 |year=1993 |pmid=8489119 |doi=] The study used blood samples to measure the patient's immune reaction to chemicals present on the surface of the "Blastocystis" cell. It found that patients diagnosed with symptomatic "Blastocystis" infection exhibited a much higher immune response than controls who had "Blastocystis" infection but no symptoms. The study was repeated in 2003 atAin Shams University in Egypt with Egyptian patients with equivalent results. .Fecal Antibody Testing: A 2003 study at Ain Shams University in Egypt indicated that patients symptomatically infected could be distinguished with a fecal antibody test. The study compared patients diagnosed with symptomatic "Blastocystis" infection to controls who had "Blastocystis" infection but no symptoms. In the group with symptoms, IgA antibodies to "Blastocystis" were detected in fecal specimens that were not present in the healthy control group.
Stool Culture: Culturing has been shown to be a more reliable method of identifying infection. In 2006, researchers reported the ability to distinguish between disease causing and non-disease causing isolates of "Blastocystis" using stool culture. cite journal |author=Tan TC, Suresh KG, Thong KL, Smith HV |title=PCR fingerprinting of Blastocystis isolated from symptomatic and asymptomatic human hosts |journal=Parasitol. Res. |volume=99 |issue=4 |pages=459–65 |year=2006 |pmid=16628457 |doi=10.1007/s00436-006-0177-0 ] "Blastocystis" cultured from patients who were sick and diagnosed with "Blastocystis" infection produced large, highly adhesive amoeboid forms in culture. These cells were absent in "Blastocystis" cultures from healthy controls. Subsequent genetic analysis showed the "Blastocystis" from healthy controls was genetically distinct from that found in patients with symptoms. Protozoal culture is unavailable in most countries due to the cost and lack of trained staff able to perform protozoal culture.
Genetic Analysis of isolates: Researchers have used techniques which allow the DNA of "Blastocystis" to be isolated from fecal specimens. This method has been reported to be more reliable at detecting "Blastocystis" in symptomatic patients than stool culture. This method also allows the species group of "Blastocystis" to be identified. Research is continuing into which species groups are associated with symptomatic (see Genetics and Symptoms)
Immuno-Fluorescence (IFA) Stain: An IFA stain causes "Blastocystis" cells to glow when viewed under a microscope, making the diagnostic method more reliable. IFA stains are in use for
Giardia andCryptosporidium for both diagnostic purposes and water quality testing. A 1991 paper from theNIH described the laboratory development of one such stain. However, no company currently offers this stain commercially.Transmission and risk factors
Humans contract "Blastocystis" infection by drinking water or eating food contaminated with
feces from an infected human or animal. cite journal
author = Tan, K.S.W.
title = "Blastocystis" in humans and animals: new insights using modern methodologies
journal = Vet. Parasitol.
volume = 126
pages = 121–144
year =1986
pmid = 15567582
doi = 10.1016/j.vetpar.2004.09.017 ] "Blastocystis" infection can be spread from animals to humans, from humans to other humans, from humans to animals, and from animals to animals. Risk factors for infection have been reported as following:* International travel: Travel to less developed countries has been cited in development of symptomatic Blastocystis infection. cite journal |author=Sohail MR, Fischer PR |title=Blastocystis hominis and travelers |journal=Travel medicine and infectious disease |volume=3 |issue=1 |pages=33–8 |year=2005 |pmid=17292002 |doi=10.1016/j.tmaid.2004.06.001 ] A 1986 study in the United States found that all individuals symptomatically infected with "Blastocystis" reported recent travel history to less developed countries. In the same study, all hospital employees working in New York who were screened for "Blastocystis" were found to have asymptomatic infections.
* Military service: Several studies have identified high rates of infection in military personnel. An early account described infection of British troops in Egypt in 1916 cite journal| journal=J. R. Army Med. Corps |author=Wenyon CM, O'Connor FW |title=An inquiry into some problems affecting the spread and incidence of intestinal protozoal infections of British troops and natives in Egypt, with special reference to the carrier question, diagnosis and treatment of amoebic dysentery, and an account of three new human intestinal protozoa |volume=28 |pages=346–67 |year=1917 ] who recovered following treatment with
emetine . A 1990 study published in "Military Medicine" from Lackland AFB in Texas concluded symptomatic infection was more common in foreign nationals, children, and immunocompromised individuals. A 2002 study published in "Military Medicine" of army personnel inThailand identified a 44% infection rate. Infection rates were highest in privates who had served the longest at the army base. cite journal |author=Leelayoova S, Rangsin R, Taamasri P, Naaglor T, Thathaisong U, Mungthin M |title=Evidence of waterborne transmission of Blastocystis hominis |journal=Am. J. Trop. Med. Hyg. |volume=70 |issue=6 |pages=658–62 |year=2004 |pmid=15211009 |doi=] A follow-up study found a significant correlation between infection and symptoms, and identified the most likely cause as contaminated water. A 2007 newspaper article suggested the infection rate of US military personnel returning from the Gulf War was 50%, quoting the head ofOregon State University 's Biomedicine department. cite news | last = Hogue | first = Theresa | title = Parasite blamed for growing number of stomach disorders | publisher = Corvallis Gazette-Times | date =January 14 ,2007 | url =http://www.gazettetimes.com/articles/2007/01/14/news/top_story/1aaa_germ.txt | accessdate = 2007-08-08 ]* Consumption of Untreated Water (well water): Many studies have linked "Blastocystis" infection with contaminated drinking water. A 1993 study of children infected symptomatically with "Blastocystis" in Pittsburgh indicated that 75% of them had a history of drinking well water or travel in less developed countries. Two studies in Thailand linked "Blastocystis" infection in military personnel and families to drinking of unboiled and untreated water. cite journal |author=Taamasri P, Mungthin M, Rangsin R, Tongupprakarn B, Areekul W, Leelayoova S |title=Transmission of intestinal blastocystosis related to the quality of drinking water |journal=Southeast Asian J. Trop. Med. Public Health |volume=31 |issue=1 |pages=112–7 |year=2000 |pmid=11023076 |doi=] A book published in 2006 noted that in an
Oregon community, infections are more common in winter months during heavy rains. . A research study published in 1980 reported bacterial contamination of well water in the same community during heavy rainfall. cite book
author = Lamka KG, LeChevallier MW, Seidler RJ.
title = Bacterial contamination of drinking water supplies in a modern rural neighborhood.
journal = Appl Environ Microbiol.
volume = 39
issue = 4
pages = 734-8
year =1980
pmid = 7377773 ] A 2007 study from China specifically linked infection with "Blastocystis sp. subtype 3" with drinking untreated water. cite journal |author=Li LH, Zhou XN, Du ZW, "et al" |title=Molecular epidemiology of human Blastocystis in a village in Yunnan province, China |journal= Parasitology International|volume= 56|issue= |pages= 281|year=2007 |pmid=17627869 |doi=10.1016/j.parint.2007.06.001 ] Recreational contact with untreated water, for example though boating, has also been identified as a risk factor . Studies have shown that "Blastocystis" survives sewage treatment plants in both the United Kingdom and Malaysia. cite journal
author = Utzinger J, Wu Z, Chen JX, Chen SH, Zhang L.
title = Viable blastocystis cysts in Scottish and Malaysian sewage samples
journal = Appl Environ Microbiol.
volume = 71
issue = 9
pages = 5619–20
year =2005
pmid = 16151162
doi = 10.1128/AEM.71.9.5619-5620.2005 ] "Blastocystis" cysts have been shown to be resistant to chlorination as a treatment method cite journal |author=Zaki M, Zaman V, Sheikh NA |title=Resistance of blastocystis hominis cysts to chlorine |journal=JPMA. The Journal of the Pakistan Medical Association |volume=46 |issue=8 |pages=178–9 |year=1996 |pmid=8936976 |doi=] and are among the most resistant cysts to ozone treatment. cite journal |author=Khalifa AM, El Temsahy MM, Abou El Naga IF |title=Effect of ozone on the viability of some protozoa in drinking water |journal=Journal of the Egyptian Society of Parasitology |volume=31 |issue=2 |pages=603–16 |year=2001 |pmid=11478459 |doi=]* Contaminated Food: Contamination of leafy vegetables has been implicated as a potential source for transmission of "Blastocystis" infection, as well as other gastrointestinal protozoa. cite journal
author = Al-Binali AM, Bello CS, El-Shewy K, Abdulla SE.
title = The prevalence of parasites in commonly used leafy vegetables in South Western, Saudi Arabia
journal = Saudi Med J.
volume = 27
issue = 5
pages = 613–6
year =2006
pmid = 16680247 ] A Chinese study identified infection with "Blastocystis sp. subtype 1" as specifically associated with eating foods grown in untreated water. cite journal
author = Li LH, Zhou XN, Du ZW, Wang XZ, Wang LB, Jiang JY, Yoshikawa H, Steinmann P, Utzinger J, Wu Z, Chen JX, Chen SH, Zhang L.
title = Molecular epidemiology of human Blastocystis in a village in Yunnan province, China
journal = Parasitol Int.
volume = 56
pages = 281
year =2007
pmid = 17627869
doi = 10.1016/j.parint.2007.06.001 ]* Daycare usage: A Canadian study identified an outbreak of "Blastocystis" associated with daycare usage. cite journal |author=Koutsavlis AT, Valiquette L, Allard R, Soto J |title=Blastocystis hominis: a new pathogen in day-care centres? |journal=Can. Commun. Dis. Rep. |volume=27 |issue=9 |pages=76–84 |year=2001 |pmid=11381629 |doi= ] Prior studies have identified outbreaks of similar protozoal infections in daycares. cite journal |author=Skeels MR, Sokolow R, Hubbard CV, Andrus JK, Baisch J.|journal=Am J Public Health. |volume=80|issue=3 |pages=305–8 |year=1990|pmid=2305910 |doi= |url = http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=2305910 |title=Cryptosporidium infection in Oregon public health clinic patients 1985-88: the value of statewide laboratory surveillance|]
* Geography: Infection rates vary geographically, and variants which produce symptoms may be less common in industrialized countries. For example, a low incidence of "Blastocystis" infection has been reported in Japan.cite journal |author=Hirata T, Nakamura H, Kinjo N, "et al" |title=Prevalence of Blastocystis hominis and Strongyloides stercoralis infection in Okinawa, Japan |journal= Parasitology Research|volume= 101|issue= |pages= 1717|year=2007 |pmid=17717704 |doi=10.1007/s00436-007-0712-7] And a study of individuals infected with "Blastocystis" in Japan found that many (43%, 23/54) carried "Blastocystis sp. subtype 2", which was found to produce no symptoms in 93% (21/23) of patients studied, in contrast to other variants which were less common but produced symptoms in 50% of Japanese individuals. Studies in urban areas of industrialized countries have found "Blastocystis" infection associated with a low incidence of symptoms. cite journal |author=Leder K, Hellard ME, Sinclair MI, Fairley CK, Wolfe R |title=No correlation between clinical symptoms and Blastocystis hominis in immunocompetent individuals |journal=J. Gastroenterol. Hepatol. |volume=20 |issue=9 |pages=1390–4 |year=2005 |pmid=16105126 |doi=10.1111/j.1440-1746.2005.03868.x ] In contrast, studies in developing countries generally show "Blastocystis" as being associated with symptoms cite journal |author=Nimri LF |title=Evidence of an epidemic of Blastocystis hominis infections in preschool children in northern Jordan |journal=J. Clin. Microbiol. |volume=31 |issue=10 |pages=2706–8 |year=1993 |pmid=8253970 |doi= ] . A higher incidence of "Blastocystis" infection has been reported in California and West Coast states. cite journal |author=Kappus KK, Juranek DD, Roberts JM |title=Results of testing for intestinal parasites by state diagnostic laboratories, United States, 1987 |journal=MMWR. CDC surveillance summaries : Morbidity and mortality weekly report. CDC surveillance summaries / Centers for Disease Control |volume=40 |issue=4 |pages=25–45 |year=1991 |pmid=1779956 |doi= ]
* Time: A 1989 study of the prevalence of "Blastocystis" in the United States found an infection rate of 2.6% in samples submitted from all 48 states. The study was part of the CDC's
MMWR Report. A more recent study in 2006 found an infection rate of 23% samples submitted from all 48 states. The more recent study was performed by a private laboratory located in the Western US, and emphasized samples from Western states which have previously been reported to have a higher infection rate.Research studies have suggested the following items are not risk factors for contracting "Blastocystis" infection:
* Consumption of municipal water near water plant not a risk factor): One study showed that municipal water was free of "Blastocystis" even when drawn from a polluted source. However, samples taken far away from the treatment plant showed cysts. The researchers suggested that aging pipes may permit intrusion of contaminated water into the distribution system. cite journal |author=Basualdo J, Pezzani B, De Luca M, Córdoba A, Apezteguía M |title=Screening of the municipal water system of La Plata, Argentina, for human intestinal parasites |journal=Int J Hyg Environ Health |volume=203 |issue=2 |pages=177–82 |year=2000 |pmid=11109572 |doi= ]
* Human-to-Human transmission among adults (not a risk factor): Some research suggests that direct human-to-human transmission is less common even in households and between married partners. One study showed different members of the same household carried different subtypes of Blastocystis. cite journal |author=Kaneda Y, Horiki N, Cheng XJ, Fujita Y, Maruyama M, Tachibana H |title=Ribodemes of Blastocystis hominis isolated in Japan |journal=Am. J. Trop. Med. Hyg. |volume=65 |issue=4 |pages=393–6 |year=2001 |pmid=11693890 |doi= ]
Prevalence
Like other protozoal infections, the prevalence of "Blastocystis" infection varies depending on the area investigated and the population selected. A number of different species groups of "Blastocystis" infect humans, cite journal |author=Noël C, Dufernez F, Gerbod D, "et al" |title=Molecular phylogenies of Blastocystis isolates from different hosts: implications for genetic diversity, identification of species, and zoonosis |journal=J. Clin. Microbiol. |volume=43 |issue=1 |pages=348–55 |year=2005 |pmid=15634993 |doi=10.1128/JCM.43.1.348-355.2005 ] with some being reported to cause disease while others do not. cite journal |author=Tan TC, Suresh KG |title=Predominance of amoeboid forms of Blastocystis hominis in isolates from symptomatic patients |journal=Parasitol. Res. |volume=98 |issue=3 |pages=189–93 |year=2006 |pmid=16323025 |doi=10.1007/s00436-005-0033-7] To date surveys have not distinguished between different types of "Blastocystis" in humans so the significance of findings may be difficult to evaluate. Developing countries have been reported to have higher incidences, however recent studies suggest that symptomatic infection with "Blastocystis" may be prevalent in certain areas of industrialized countries as well:
* A nation-wide study conducted by the CDC using data reported from 1987 found the prevalence "Blastocystis" infection in the United States to be 2.6%. The study indicated that Western states, such as California, reported a higher prevalence.
* A 2000 study by a private laboratory of stool samples from 48 states in the United States identified a prevalence of 23%. cite journal |author=Amin OM |title=Seasonal prevalence of intestinal parasites in the United States during 2000 |journal=Am. J. Trop. Med. Hyg. |volume=66 |issue=6 |pages=799–803 |year=2002 |pmid=12224595 |doi= ] The study was conducted by a laboratory in Arizona and emphasized Western states which have previously been found to have higher rates of "Blastocystis" infection.
* A Canadian study of samples received in 2005 identified "Blastocystis" as the most prevalent protozoal infection identified. cite journal |author=Lagacé-Wiens PR, VanCaeseele PG, Koschik C |title=Dientamoeba fragilis: an emerging role in intestinal disease |journal=CMAJ : Canadian Medical Association journal journal de l'Association medicale canadienne |volume=175 |issue=5 |pages=468–9 |year=2006 |pmid=16940260 |doi=10.1503/cmaj.060265]
* A study in Pakistan identified "Blastocystis" infection in 7% of the general population and 46% of patients with irritable bowel syndrome. The study used stool culture for identification.cite journal |author=Yakoob J, Jafri W, Jafri N, "et al" |title=Irritable bowel syndrome: in search of an etiology: role of Blastocystis hominis |journal=Am. J. Trop. Med. Hyg. |volume=70 |issue=4 |pages=383–5 |year=2004 |pmid=15100450 |doi=]
Phylogenetics and symptoms
Physicians have produced conflicting reports regarding whether "Blastocystis" causes disease in humans. These reports resulted in a brief debate in medical journals in the early 1990s between some physicians in the United States who believed that "Blastocystis" was harmless, and physicians in the United States and overseas who believed it could cause disease.
At the time, it was common practice to identify all "Blastocystis" from humans as "
Blastocystis hominis ", while "Blastocystis" from animals was identified differently (i.e. "Blastocystis ratti" from rats). Research performed since then has shown that the concept of "Blastocystis hominis" as a unique species of "Blastocystis" infecting humans is not supported by microbiological findings. Although one species group associated with primates was found, it was also discovered that humans can acquire infection from any one of nine species groups of "Blastocystis" which are also carried by cattle, pigs, rodents, chickens, pheasants, monkeys, dogs and other animals. Research has suggested that some types produce few or no symptoms, while others producing illness and intestinal inflammation. Researchers have suggested conflicting reports may be due to the practice of naming all "Blastocystis" from humans "Blastocystis hominis" and have proposed discontinuing the use of that term.A standard naming system for "Blastocystis" organisms from humans and animals has been proposed which names "Blastocystis" isolates according to the genetic identity of the "Blastocystis" organism rather than the host. The naming system used identifies all isolates as "Blastocystis sp. subtype nn" where nn is a number from 1 to 9 indicating the species group of the "Blastocystis" organism. The identification of the species can not be performed with a microscope at this time, because the different species look alike. Identification requires equipment for genetic analysis that is common in microbiology laboratories, but not available to most physicians. Some new scientific papers have begun using the standard naming system. cite journal |author=Menounos PG, Spanakos G, Tegos N, Vassalos CM, Papadopoulou C, Vakalis NC |title=Direct detection of Blastocystis sp. in human faecal samples and subtype assignment using single strand conformational polymorphism and sequencing |journal= Molecular and Cellular Probes|volume= 22|issue= |pages= 24|year=2007 |pmid=17669623 |doi=10.1016/j.mcp.2007.06.007]
The following researchers have reported findings that suggest that different types of "Blastocystis" cause different manifestations in humans:
# A German researcher, Dr. Kukoschke, was one of the first researchers to suggest that different species of "Blastocystis" were present in symptomatic and asymptomatic individuals. In a 1992 study, he noted that isolates from sick patients with "Blastocystis" would not grow in human serum, but rather required rabbit or horse serum to grow. cite journal |author=Kukoschke KG, Müller HE |title=Varying incidence of Blastocystis hominis in cultures from faeces of patients with diarrhoea and from healthy persons |journal=Zentralbl. Bakteriol. |volume=277 |issue=1 |pages=112–8 |year=1992 |pmid=1520961 |doi= ] Isolates from symptomatic individuals would not grow well in human serum, but required horse serum instead.
# In 1993, Dr. Charles Zierdt, anNIH researcher, used a serum antibody test in study of individuals infected with "Blastocystis." He compared the results from subjects with symptoms to those who were healthy. His 1993 publication showed that the subjects with symptoms had much higher levels of antibodies to "Blastocystis" in blood samples, and that a dividing line could be drawn separating the two groups. At this time a similar finding had been made relative to "Entamoeba histolytica ", and researchers were developing methods to distinguish between the pathogenic "Entamoeba histolytica " species, and the harmless "Entamoeba dispar " species. In his paper, he drew a parallel to the research into that protozoan.
# A 1994 study Dr. DW MacPherson of St. Joseph's Hospital in Canada noted variation in cyst forms and suggested different species were present. cite journal |author=MacPherson DW, MacQueen WM |title=Morphological diversity of Blastocystis hominis in sodium acetate-acetic acid-formalin-preserved stool samples stained with iron hematoxylin |journal=J. Clin. Microbiol. |volume=32 |issue=1 |pages=267–8 |year=1994 |pmid=7510311 |doi= ]
# A 1999 study by Dr. M Lanuza, et al of the University of Valencia, Spain found that the protein profiles exhibited in "Blastocystis" cultures from symptomatic patients differed from those of patients without symptoms. cite journal |author=Lanuza MD, Carbajal JA, Villar J, Mir A, Borras R. |title=Soluble-protein and antigenic heterogeneity in axenic Blastocystis hominis isolates: pathogenic implications|journal=Parasitol Res.|volume=85|issue=2 |pages=93–7 |year=1999 |pmid=9934956 |doi=]
# In 2003, Zierdt's serum antibody research results were repeated by Dr. Mahmoud at Aga Khan University in Egypt.
# In 2006, researchers at the University of Malaysia reported that isolates from symptomatic individuals produced large amoeboid forms when cultured in the presence of bacteria. These forms were absent from isolates cultured from healthy carriers. The study noted a 100% association which had not been found previously, and suggested that previous studies had not cultured the organisms long enough, as at least 4 days were required for some cultures to produce amoeboid forms. The group also performed genetic analysis of isolates from symptomatic individuals and found they belonged to a narrow genetic group, while isolates from asymptomatic carriers were found to be from a genetically diverse clade.
# A 2006 study performed by Dr. Rune Stensvold with patients being diagnosed in Denmark identified "Blastocystis sp. subtypes 2, 3 and 4" in most patients being diagnosed for diarrhea.Pathogeneses (how it causes disease)
Pathogenesis refers to the mechanism by which an organism causes disease. The following disease-causing mechanisms have been reported in studies of "Blastocystis" infection:
* Barrier Disruption: In isolates from "Blastocystis sp. subtype 4", study has demonstrated that "Blastocystis" has the ability to alter the arrangement of F-actin in intestinal epithelial cells. Actin filaments are important in stabilizing
tight junctions ; they in turn stabilize the barrier, which is a layer of cells, between the intestinal epithelial cells and the intestinal content. cite journal |author=Puthia MK, Sio SW, Lu J, Tan KS |title=Blastocystis ratti induces contact-independent apoptosis, F-actin rearrangement, and barrier function disruption in IEC-6 cells |journal=Infect. Immun. |volume=74 |issue=7 |pages=4114–23 |year=2006 |pmid=16790785 |doi=10.1128/IAI.00328-06 ] The parasite causes the actin filaments to rearrange, and so compromising barrier function. This has been suggested to contribute to the diarrheal symptoms sometimes observed in "Blastocystis" patients.* Invasiveness: Invasive infection has been reported in humans cite journal |author=al-Tawil YS, Gilger MA, Gopalakrishna GS, Langston C, Bommer KE |title=Invasive Blastocystis hominis infection in a child |journal=Archives of pediatrics & adolescent medicine |volume=148 |issue=8 |pages=882–5 |year=1994 |pmid=8044274 |doi= ] and animal studies.
* Immune Modulation: "Blastocystis" has been shown to provoke cells from the human colon to produce inflammatory
cytokines Interleukin-8 andGM-CSF . cite journal |author=Long HY, Handschack A, König W, Ambrosch A |title=Blastocystis hominis modulates immune responses and cytokine release in colonic epithelial cells |journal=Parasitol. Res. |volume=87 |issue=12 |pages=1029–30 |year=2001 |pmid=11763434 |doi= ]Interleukin-8 plays a role in rheumatoid arthritis.* Protease Secretion: "Blastocystis" secretes a
protease that breaks up antibodies produced and secreted into thegastrointestinal tract lumen. cite journal |author=Puthia MK, Vaithilingam A, Lu J, Tan KS |title=Degradation of human secretory immunoglobulin A by Blastocystis |journal=Parasitol. Res. |volume=97 |issue=5 |pages=386–9 |year=2005 |pmid=16151742 |doi=10.1007/s00436-005-1461-0 ] These antibodies, known as immunoglobulin A (IgA), make up the immune defense system of human by preventing the growth of harmful microorganisms in the body and by neutralizingtoxin s secreted by these microorganisms. By breaking up the antibodies, it allows the persistence of "Blastocystis" in the human gut. Another more recent study has also shown and proposed that, in response to the proteases secreted by "Blastocystis", the intestinal host cells would signal a series of events to be carried out, eventually leading to the self-destruction of the host cells – a phenomenon known asapoptosis * Other secretory mechanism: A study of a different protozoan which produces similar symptoms, "
Entamoeba histolytica ", found that organism secretes several neurologically active chemicals, such asserotonin andSubstance P . cite journal |author=McGowan K, Kane A, Asarkof N, "et al" |title=Entamoeba histolytica causes intestinal secretion: role of serotonin |journal=Science |volume=221 |issue=4612 |pages=762–4 |year=1983 |pmid=6308760 |doi= ] cite journal |author=McGowan K, Guerina V, Wicks J, Donowitz M |title=Secretory hormones of Entamoeba histolytica |journal=Ciba Found. Symp. |volume=112 |issue= |pages=139–54 |year=1985 |pmid=2861068 |doi= ] Serum levels ofserotonin have been found to be elevated in patients with "Entamoeba histolytica ". [cite journal |author=Banu, Naheed, et al. |title=Neurohumoral alterations and their role in amoebiasis |journal=Indian J. Clin Biochem |volume=20 |issue=2 |pages=142–5 |year=2005 |url=http://medind.nic.in/iaf/t05/i2/iaft05i2p142.pdf |doi=10.1007/BF02867414|format=PDF] One paper noted the diffuse symptoms of "Blastocystis" infection correllate withserotonin 's role in the body, and suggested a similar mechanism may be present in "Blastocystis" infection.cite journal |author=Boorom KF |title=Is this recently characterized gastrointestinal pathogen responsible for rising rates of inflammatory bowel disease (IBD) and IBD associated autism in Europe and the United States in the 1990s? |journal=Med. Hypotheses |volume=69 |issue=3 |pages=652–9 |year=2007 |pmid=17382484 |doi=10.1016/j.mehy.2007.01.027]Association with (IBS) and other disease
The following reports have linked "Blastocystis" infection to
Irritable bowel syndrome ::*A study of IBS patients in the Middle East found 46% were infected with "Blastocystis" vs. 7% of healthy controls. :*An additional study of IBS patients in the Middle East showed a "significantly increased" immune reaction in IBS patients to "Blastocystis", even when the organism could not be identified in stool samples. cite journal |author=Hussain R, Jaferi W, Zuberi S, "et al" |title=Significantly increased IgG2 subclass antibody levels to Blastocystis hominis in patients with irritable bowel syndrome |journal=Am. J. Trop. Med. Hyg. |volume=56 |issue=3 |pages=301–6 |year=1997 |pmid=9129532 |doi= ] :*A European study compared "Blastocystis" infection rates in IBS patients to those of healthy controls and found a statistically significant infection rate in IBS patients. cite journal |author=Giacometti A, Cirioni O, Fiorentini A, Fortuna M, Scalise G |title=Irritable bowel syndrome in patients with Blastocystis hominis infection |journal=Eur. J. Clin. Microbiol. Infect. Dis. |volume=18 |issue=6 |pages=436–9 |year=1999 |pmid=10442423 |doi= ] :*Early reports from the US physicians in the 1980's suggested the presence of the organism was not relevant to the diagnostic process, and patients infected with "Blastocystis" could be diagnosed with IBS. cite journal |author=Markell EK, Udkow MP |title=Blastocystis hominis: pathogen or fellow traveler? |journal=Am. J. Trop. Med. Hyg. |volume=35 |issue=5 |pages=1023–6 |year=1986 |pmid=3766850 |doi=]
The following reports have linked "Blastocystis" infection to
inflammatory bowel disease : :* A study using riboprinting identified specific types of "Blastocystis" as associated with inflammation. :* A case report described inflammatory bowel disease in conjunction with "Blastocystis" infection. :* Three research groups have reported experimental infection of mice with "Blastocystis" produces intestinal inflammation. :* An article in a non-peer reviewed medical journal noted that the increase in "Blastocystis" case reports coincided with reported increases in the prevalence ofinflammatory bowel disease from several European countries .References
External links
* [http://www.cdc.gov/ncidod/dpd/parasites/blastocystishominis/default.htm CDC description of Blastocystis hominis]
* [http://www.bhomcenter.org Blastocystis Research Foundation]
Wikimedia Foundation. 2010.
