- Babesiosis
DiseaseDisorder infobox
Name = Babesiosis
Caption =
ICD10 = ICD10|B|60|0|b|50
ICD9 = ICD9|088.82
ICDO =
OMIM =
DiseasesDB = 1200
MedlinePlus =
eMedicineSubj =
eMedicineTopic =
MeshID = D001404Babesiosis is a malaria-like
parasitic disease caused by "Babesia ", agenus ofprotozoa l piroplasms.cite journal |author=Herwaldt BL, Persing DH, Précigout EA, et al. |title=A fatal case of babesiosis in Missouri: Identification of another piroplasm that infect humans |journal=Annals of Internal Medicine|volume=124 |issue=7 |pages=643–650 |year=1996 [http://annals.highwire.org/cgi/content/abstract/124/7/643] ] Aftertrypanosome s, "Babesia" are thought to be the second most common bloodparasite s of mammals and they can have a major impact on health of domestic animals in areas without severe winters. Human babesiosis is uncommon, but reported cases have risen recently because of expanded medical awareness.cite journal |author=Hunfeld KP, Hildebrandt A, Gray JS |title=Babesiosis: Recent insights into an ancient disease |journal=Int J Parasitol |volume=38 |issue=11 |pages=1219-37 |year=2008 |doi=10.1016/j.ijpara.2008.03.001]Terminology
The disease is named for the genus of the causative organism, [ [http://mw4.m-w.com/dictionary/babesia "babesia"] at Merriam-Webster online.] which was in turn named after the bacteriologist
Victor Babeş . [ [http://www.whonamedit.com/doctor.cfm/367.html Victor Babeş] at whonamedit.com] Equine babesiosis is also known as piroplasmosis.Epidemiology
Babesiosis is a vector-borne illness usually transmitted by Ixodid
tick s. "Babesia microti" uses the same tick vector, "Ixodes scapularis ", asLyme disease andehrlichiosis , and may occur in conjunction with these other diseases. In endemic areas, the organism can also be transmitted byblood transfusion . In North America, the disease exists mostly in eastern Long-Island and its barrier island,Fire Island , and the islands off the coast of Massachusetts.Fact|date=August 2008 It is sometimes called "The Malaria of The Northeast."Cases of babesiosis have been reported in a wide range of European countries. Disease in Europe is usually due to infection with "Babesia divergens", while in the United States "Babesia microti" is the species most commonly associated with human disease. Babesiosis has also been observed in
Korea .cite journal |author=Kim JY, Cho SH, Joo HN, "et al" |title=First case of human babesiosis in Korea: detection and characterization of a novel type of Babesia sp. (KO1) similar to ovine babesia |journal=J. Clin. Microbiol. |volume=45 |issue=6 |pages=2084–7 |year=2007 |month=June |pmid=17392446 |pmc=1933034 |doi=10.1128/JCM.01334-06 |url=http://jcm.asm.org/cgi/pmidlookup?view=long&pmid=17392446]Most cases of babesia infection are asymptomatic or include mild fevers and anemia and go unnoticed. In more severe cases, there are symptoms similar to malaria, with fevers up to 105°F / 40°C, shaking chills, and severe anemia (hemolytic anemia). Organ failure may follow including adult respiratory distress syndrome. Severe cases occur mostly in people who have had their spleen removed surgically. Severe cases are also more likely to occur in the very young, very old, and persons with
immunodeficiency , such asHIV/AIDS patients. Some people with babesiosis have additional tick-borne illnesses.A reported increase in babesiosis diagnoses in recent years is thought to be caused by more widespread testing and higher numbers of people with immunodeficiencies coming in contact with ticks, the disease vector.
Little is known about the occurrence of "Babesia" species in malaria-endemic areas, where "Babesia" can easily be misdiagnosed as "
Plasmodium ".Pathophysiology
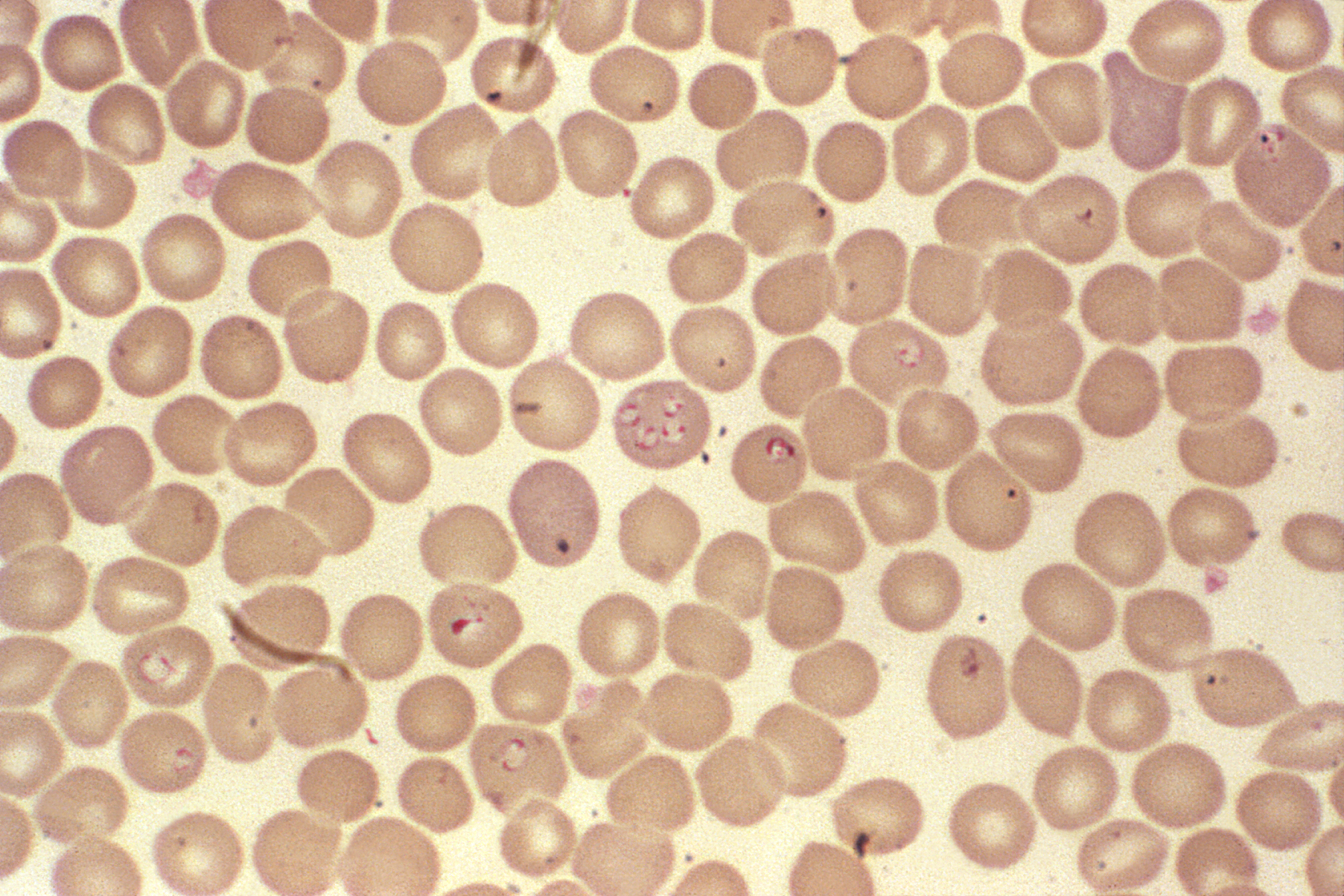
"Babesia" parasites reproduce in
red blood cell s, where they can be seen as cross-shaped inclusions (4merozoite s asexually budding but attached together forming a structure looking like a "Maltese Cross ") cite journal | author =Noskoviak K, Broome E. | title = Images in clinical medicine. Babesiosis | journal = N Engl J Med. | volume = 358 | issue = 17 | pages = e19 | year = 2008 | pmid = 18434647 | doi =10.1056/NEJMicm070903 ] and causehemolytic anemia , quite similar tomalaria .Note that unlike the "
Plasmodium " parasites that cause malaria, "Babesia" species lack an exo-erythrocytic phase, so the liver is usually not affected.In animals "Babesia canis rossi", "Babesia bigemina", and "Babesia bovis" cause particularly severe forms of the disease that include a severe haemolytic anaemia, with positive erythrocyte-in-saline-agglutination test indicating an immune mediated component to the haemolysis. Common sequelae include haemoglobinuria "red-water", disseminated intravascular coaguation (DIC) and "cerebral babesiosis" caused by sludging of erythrocytes in cerebral capilaries.
Diagnosis
A high index of suspicion is necessary to diagnose babesiosis. Babesiosis develops only in patients who live in or travel to an endemic area or receive a contaminated
blood transfusion within the preceding 9 weeks, so this aspect of the medical history is vital. Babesiosis may be suspected when a person with such an exposure history develops persistent fevers and hemolytic anemia. The definitive diagnostic test for babesiosis is the identification of parasites on a Giemsa-stained thin blood smear.cite journal |author=Wormser GP, Dattwyler RJ, Shapiro ED, "et al" |title=The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America |journal=Clin. Infect. Dis. |volume=43 |issue=9 |pages=1089–134 |year=2006 |month=November |pmid=17029130 |doi=10.1086/508667 |url=] So-called "Maltese cross formations" on the blood film are essentially diagnostic of babesiosis, since they are not seen in malaria, the primary differential diagnosis. Careful examination of multiple blood smears may be necessary, since "Babesia" may infect less than 1% of circulating red blood cells and thus be easily overlooked.cite journal |author=Krause PJ |title=Babesiosis diagnosis and treatment |journal=Vector Borne Zoonotic Dis. |volume=3 |issue=1 |pages=45–51 |year=2003 |pmid=12804380 |doi=10.1089/153036603765627451 |url=]Serologic testing for antibodies against "Babesia" (both
IgG andIgM ) can detect low-level infection in cases where there is a high clinical suspicion but negative blood film examinations. Serology is also useful for differentiating babesiosis frommalaria in cases where people are at risk for both infections. Since detectable antibody responses require approximately one week after infection to develop, serologic testing may be falsely negative early in the disease course. [cite journal |author=Krause PJ, Telford SR, Ryan R, "et al" |title=Diagnosis of babesiosis: evaluation of a serologic test for the detection of Babesia microti antibody |journal=J. Infect. Dis. |volume=169 |issue=4 |pages=923–6 |year=1994 |month=April |pmid=8133112 |doi= |url=]A
polymerase chain reaction (PCR) test has been developed for the detection of "Babesia" from the peripheral blood. [cite journal |author=Persing DH, Mathiesen D, Marshall WF, "et al" |title=Detection of Babesia microti by polymerase chain reaction |journal=J. Clin. Microbiol. |volume=30 |issue=8 |pages=2097–103 |year=1992 |month=August |pmid=1500517 |pmc=265450 |doi= |url=http://jcm.asm.org/cgi/pmidlookup?view=long&pmid=1500517] PCR may be at least as sensitive and specific as blood film examination in diagnosing babesiosis, though it is also significantly more expensive. [cite journal |author=Krause PJ, Telford S, Spielman A, "et al" |title=Comparison of PCR with blood smear and inoculation of small animals for diagnosis of Babesia microti parasitemia |journal=J. Clin. Microbiol. |volume=34 |issue=11 |pages=2791–4 |year=1996 |month=November |pmid=8897184 |pmc=229405 |doi= |url=http://jcm.asm.org/cgi/pmidlookup?view=long&pmid=8897184] Most often, PCR testing is used in conjunction with blood film examination and possibly serologic testing.Other laboratory findings include decreased numbers of
red blood cells andplatelets oncomplete blood count .In Animals Babesiosis is suspected by observation of clinical signs (haemoglobinuria and anaemia) in animals in endemic areas. Diagnosis is confirmed by observation of merozoites on thin film blood smear examined at maximum magnification under oil using Romonovski stains (methylene blue and eosin). This is a routine part of the veterinary examination of dogs and ruminants in regions where babesiosis is endemic.
"Babesia canis" and "Babesia bigemina" are "large babesias" that form paired merozoites in the erythrocytes , commonly described as resembling "two pears hanging together", rather than the "Maltese Cross" of the "small babesias". Their merozoites are approximately twice the size of small babesias.
Cerebral babesiosis is suspected in-vivo when neurological signs (often severe) are seen in cattle that are positive for babesia bovis on blood smear. Outspoken red discolouration of the grey matter on post-mortem further strengthens suspicion of cerebral babesiosis. Diagnosis is confirmed post-mortem by observation of babesia infected erythrocytes sludged in the cerebral cortical capilaries in a brain smear.
Treatment
Most cases of babesiosis resolve without any specific treatment. For ill patients, treatment is usually a two-drug regimen. The regimen of
quinine andclindamycin has been used,cite journal |author=Setty S, Khalil Z, Schori P, Azar M, Ferrieri P |title=Babesiosis. Two atypical cases from Minnesota and a review |journal=Am. J. Clin. Pathol. |volume=120 |issue=4 |pages=554–9 |year=2003 |month=October |pmid=14560566 |doi=10.1309/N3DP-9MFP-NUJD-4XJY |url=http://ajcp.metapress.com/openurl.asp?genre=article&issn=0002-9173&volume=120&issue=4&spage=554] but is often poorly tolerated; recent evidence suggests that a regimen ofatovaquone andazithromycin can be equally effective cite journal | author = Krause P, Lepore T, Sikand V, Gadbaw J, Burke G, Telford S, Brassard P, Pearl D, Azlanzadeh J, Christianson D, McGrath D, Spielman A | title = Atovaquone and azithromycin for the treatment of babesiosis | journal = N Engl J Med | volume = 343 | issue = 20 | pages = 1454–8 | year = 2000 | pmid = 11078770 | doi = 10.1056/NEJM200011163432004] . In life-threatening cases, exchange transfusion is performed. In this procedure, the infected red blood cells are removed and replaced with fresh ones.Veterinary treatment of Babesiosis does not normally use antibiotics. In animals diminazene (Berenil), imidocarb or trypan blue would be the drugs of choice for treatment of "Babesia canis rossi" (Dogs in Africa), "Babesia bovis", and "Babesia bigemina" (cattle in Southern Africa).
There is a vaccine that is effective against "Babesia canis canis" (dogs in the mediterranean region) but this is ineffective against "Babesia canis rossi". "Babesia imitans" casuses a mild form of the disease that frequently resolves without treatment (dogs in South East Asia).
References
External links
* http://www.dpd.cdc.gov/dpdx/HTML/Babesiosis.htm -
Public domain source from which the first version of this article was derived.
Wikimedia Foundation. 2010.
